Bladder injury after blunt trauma is relatively uncommon, but needs to be identified promptly. Nearly every patient (97%+) with a bladder injury will have hematuria that is visible to the naked eye. This should prompt the trauma professional to obtain a CT of the abdomen/pelvis and a CT cystogram.
The CT of the abdomen and pelvis will identify any renal or ureteral (extremely rare!) source for the hematuria. The CT cystogram will demonstrate a bladder injury, but only if done properly!
During most trauma CT scanning of the abdomen and pelvis, the bladder is allowed to passively fill, either by having no urinary catheter and having the patient hold it, or by clamping the catheter if it is present. Unfortunately, this does not provide enough pressure to demonstrate small intraperitoneal bladder injuries and most extraperitoneal injuries.
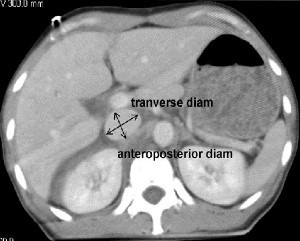
The proper technique involves infusing contrast into the bladder through a urinary catheter. At least 350cc of dilute contrast solution must be instilled for proper distension and accurate diagnosis. This can be done prior to the abdominal scan. Once the initial scan has been obtained, the bladder must be emptied and a focused scan of just the bladder should be performed (post-void images). Several papers have shown that this technique is as accurate as conventional retrograde cystography, with 100% sensitivity and specificity for intraperitoneal ruptures. The sensitivity for extraperitoneal injury was slightly less at 93%.
Bottom line: Gross hematuria equals CT of the abdomen/pelvis and a proper CT cystogram, as described above. Don’t try to cheat and passively fill the bladder. You will miss about half of these injuries!
Related posts:
Reference: CT cystography with multiplanar reformation for suspected bladder rupture: experience in 234 cases. Am J Roentgenol 187(5):1296-302, 2006.

Intraperitoneal bladder rupture

Extraperitoneal bladder injury