What goes around comes around. Fifty plus years ago, the only transfusion product available was whole blood. Then the major blood banks discovered that more patients could be treated for specific problems if the blood were fractionated. Packed red cells then became the standard for trauma transfusion and persists to this day.
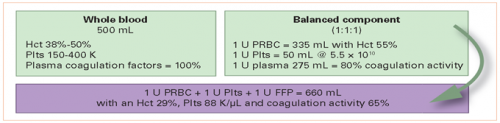
But there is a move afoot to re-explore the use of whole blood. There are many theoretical advantages, since our trauma patients are bleeding whole blood, not packed cells. Unfortunately, combining a unit of packed red cells, plasma, and platelets does not give you a reconstituted unit of whole blood by a long shot. Check out this diagram:
The challenge is that we are used to only thinking about universal donor red cells (group O Rh-). This is the safest packed cell product to give a patient with an unknown blood type. But unfortunately, it is also one of the hardest to find, present in about 7% of the population.
Packed red cells are nearly plasma free. What we don’t think about with whole blood is the level of antibodies to blood groups that are present in the plasma. Group O blood will have plasma with anti-A and anti-B antibodies. So if we include the plasma with those universal donor red cells, these antibodies may attack the patient’s red cells if he or she is group A, B, or AB and cause a reaction.
Theoretically, this issue can be avoided by using universal donor plasma (group AB+). Since the donor has all of the major group antigens, they will have no antibodies in their plasma. Unfortunately again, this is a rare type and tough to get donors (about 3% of the population).
To avoid potential transfusion reactions, group O whole blood is tested for antibody titers, and only low titer blood is selected for transfusion. Typically Rh- whole blood has been selected to avoid any issues with Rh incompatibility, even though reactions to this antigen are usually mild.
The group at the University of Texas – Houston reviewed their experience using Rh+ low titer group O blood in trauma resuscitations. Their two-year study substituted Rh+ whole blood when Rh- product was not available. They monitored patients for transfusion reactions, renal failure, sepsis, VTE, and ARDS.
Here are the factoids:
- A total of 637 patients received low titer group O blood during the study period; 448 received Rh+ product and 189 received Rh-
- Those receiving Rh+ blood were more likely to be male, had lower initial SBP, and a significantly lower GCS (7 vs 12)
- Overall there were no differences in hemolysis labs, transfusion reaction, complications or mortality
- The patient groups were then sliced and diced by their own Rh antibody status to see if Rh- patients had an increased likelihood of problems from Rh+ plasma
- Once again, the Rh- subgroup was significantly different for sex (57% female vs 26% in the Rh+ group), and blunt trauma mechanism (92% vs 70%)
- And once again no differences were seen in hemolysis, transfusion reaction, complications or mortality
The authors then concluded that Rh+ low titer whole blood is a safe alternative in either Rh+ or Rh- patients.
My comments: Sounds good, right? But wait a minute! This was a non-randomized observational study. It appears that Rh+ whole blood was used when Rh- was unavailable, which was quite a bit of the time. This is clear when you see the demographic differences listed above between the two recipient groups, as well as the subgroups stratified by their own Rh status.
This is the first thing that makes me a bit more skeptical of the recommendation. The other one is something you’ve heard me harp about before… non-inferiority studies. This abstract tries to say that since they did not detect a difference, then the two products are equivalent.
That is only true if there is adequate power in the number of patients studied. If not, you may not be able to show a statistically significant difference. By my own calculations, if the incidence of transfusion reaction in the Rh- group is 1% and the ratio of the patient groups is 0.42, the reported sample size could only show a significant difference if the Rh+ patients had a 5% transfusion reaction rate.
So is it truly non-inferior, or does the study need include a lot more patients?
Here are my questions for the authors and presenter:
- What is the impact of the non-randomized patient selection process on your results? The groups and subgroups appear to be very different. Couldn’t this influence your results?
- Exactly what type of statistical analysis did you use? Your abstract merely lists the software package, not the specific tests applied.
- Do you believe that your study is sufficiently powered? What assumptions did you use to calculate this?
As we move toward more use of whole blood, the Rh question will be an important one. I look forward to questioning the authors on this one!
Reference: Can Rh+ whole blood be safely used as an alternative to Rh- product? An analysis of efforts to improve the sustainability of a hospital’s low titer group O whole blood program. EAST 2021, Paper 17.