This is a fairly common question from victims of gunshots and their families. As you know, bullets are routinely left in place unless they are superficial. It may cause more damage to try to extract one, especially if it has come to rest in a deep location. But is there danger in leaving the bullet alone?
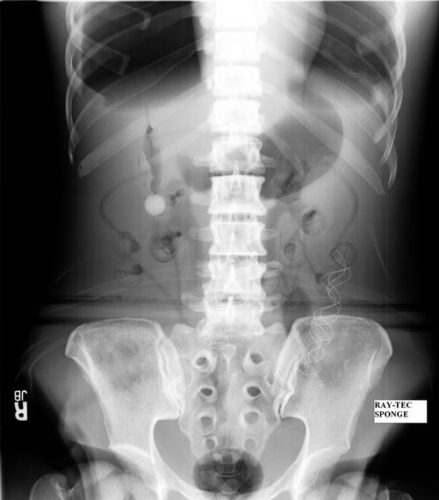
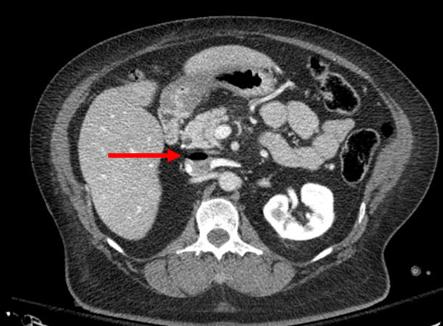
One of the classic papers on this topic was published in 1982 by Erwin Thal at Parkland Hospital in Dallas. The paper recounted a series of 16 patients who had developed signs and symptoms of lead poisoning (plumbism) after a gunshot or shotgun injury. The common thread in these cases was that the injury involved a joint or bursa near a joint. In some cases the missile passed through the joint/bursa but came to rest nearby, and a synovial pseudocyst formed which included the piece of lead. The joint fluid bathing the projectile caused lead to leach into the circulation.
The patients in the Parkland paper developed symptoms anywhere from 3 days to 40 years after injury. As is the case with plumbism, symptoms were variable and nonspecific. Patients presented with abdominal pain, anemia, cognitive problems, renal dysfunction and seizures to name a few.

Bottom line: Any patient with a bullet or lead shot that is located in or near a joint or bursa should have the missile(s) promptly and surgically removed. Any lead that has come to rest within the GI tract (particularly the stomach) must be removed as well. If a patient presents with odd symptoms and has a history of a retained bullet, obtain a toxicology consult and begin a workup for lead poisoning. If levels are elevated, the missile must be extracted. Chelation therapy should be started preop because manipulation of the site may further increase lead levels. The missile and any stained tissues or pseudocyst must be removed in their entirety.
Granted, this is a very old paper. Over the years, a few papers on the topic have popped up from time to time. In my next post, I’ll review a meta-analysis on this topic that was published just last year.
Reference: Lead poisoning from retained bullets. Ann Surg 195(3):305-313, 1982.