Decades ago, intubation of trauma patients only took place in the operating room, and only anesthesiologists performed it. As the discipline of Emergency Medicine came into being in the 1980s, emergency physicians became skilled in this procedure. Occasional trauma intubations had to occur in the ED, and typically anesthesia was called for it.
As the emergency physicians became more comfortable and improved their skills, they also started intubating. I distinctly remember a paper from the time (which I unfortunately do not have a reference to) stating that ED and OR intubation were equally safe if the ED intubation field could be made to look like the OR. This thinking has become commonplace, and in most trauma centers, intubation is now provided nearly exclusively by emergency physicians. Anesthesia is called only for extremely difficult cases.
But we have all been involved in cases where the patient is severely injured, usually hypotensive, and crashes and burns during or immediately after the procedure. This is likely due to a combination of loss of sympathetic tone due to the drugs administered, increased vagal tone from instrumenting the airway, and hypovolemia.
Authors from the University of Wisconsin, University of Pennsylvania, and Johns Hopkins hypothesized that ED intubation for patients requiring urgent operation for hemorrhage control was associated with adverse outcomes. They performed a three-year registry study from the National Trauma Program Databank of patients requiring laparotomy for hemorrhage control within 60 minutes of arrival. They excluded the dead and nearly dead (DOA, ED thoracotomy) and patients with immediate indications for intubation (head, neck, or facial trauma). They compared mortality, ED dwell time, blood transfusions, and major complications between patients with ED vs. OR intubation.
Here are the factoids:
- Nearly 10,000 patients from 253 Level I or II trauma centers were included in the study
- About 20% of patients underwent intubation in the ED, and they were more likely to have blunt trauma mechanism and higher ISS (22 vs. 17)
- Initial vital signs were not clinically significant between the ED and OR groups
- Mortality in the ED group was significantly higher (17% vs. 7%), the ED dwell time was significantly longer ( 31 vs. 22 minutes), required significantly more blood transfusion (6 vs. 4 units), and had a significantly higher risk of major complications (specifically cardiac arrest, AKI, and ARDS)
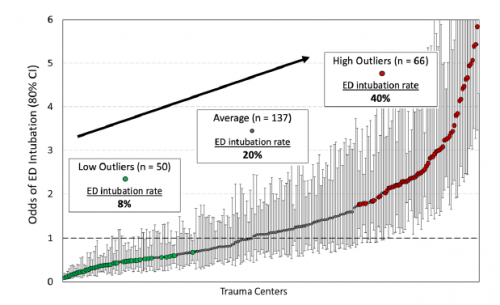
- There was a wide variation in the rate of ED intubation across all the hospitals. Centers with the highest rate of ED intubations were 5x more likely to intubate than the lowest rate centers. The patient case mix could not explain this difference.
- The lower ED intubation rate hospitals tended to be nonprofit Level I university hospitals
- Centers with high levels of hemorrhage control surgery were more likely to intubate in the OR
Bottom line: From a purely technical perspective, the old dogma about patient location not making a difference is basically true. The process of getting an airway safely into the patient and secured is equivalent wherever it is done as long as the lighting, equipment, and skill levels are equivalent.
But when one considers the physiologic aftermath of this process, things are obviously more nuanced. Actively bleeding patients are extremely challenged, down to their organ and cellular levels. Disrupting their normal compensatory mechanisms is clearly associated with a significant downside.
We should clearly distinguish the patient who needs an airway for airway’s sake or cerebral protection from one who needs to be in the OR for bleeding control. Other papers have shown that mortality increases as each minute ticks by in the hemorrhaging patient. Trauma programs need to monitor these patients and do a performance improvement deep dive into all trauma patients intubated in the ED to ensure appropriate decision-making.
Reference: Emergency Department Versus Operating Room Intubation of Patients Undergoing Immediate Hemorrhage Control Surgery. Journal of Trauma and Acute Care Surgery, Publish Ahead of Print
DOI: 10.1097/TA.0000000000003907