Patients with severe head injury need all the help they can get. Mannitol is one tool that is time-tested and cheap. But how do you decide who gets it and when?
Mannitol is a powerful osmotic diuretic that pulls extracellular water from everywhere, including the brain. By reducing the size of the brain overall, it drops pressure inside the skull (ICP) somewhat.
Mannitol can be used anytime during the acute phase of trauma care for three indications in patients with head trauma:
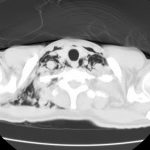
- Focal neurologic deficit. This is due to transtorial herniation, and may manifest clinically as unilateral pupil dilation or hemiparesis. It may also be seen on CT scan.
- Progressive neurologic deterioration. This is typical of rising ICP and can be diagnosed when your previously talking patient becomes lethargic.
- Clinical evidence of high ICP. This is the Cushing response (hypertension with bradycardia). Do not treat this hypertension with other meds, it is a brain protective mechanism!
The literature does not have any good studies that show effectiveness or survival benefit. However, most trauma professionals have seen the dramatic improvement in neurologic status that can occur after early administration.
Bottom line: Mannitol is cheap and it works! Consider it early if any of the three indications above are seen. And don’t forget to put a urinary catheter in immediately because the diuresis that it causes is impressive. And no studies thus far have been able to prove that hypertonic saline is any better or worse than mannitol.