What The Heck Is It? Final Answer!
Yesterday, I posted the physical exam findings on this mystery object. A tiny puncture wound was present just to the right of the xiphoid on the lower chest wall, and a small sharp point was palpable.
Here’s how to deal with it:
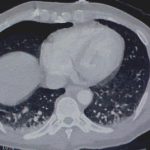
Step 1. (Image 1) Don’t let it move or try to pull it out immediately! I didn’t want this thing to go in any further, or work it’s way out in case it was in the heart. I snapped a hemostat on the end of it for stabilization.
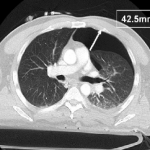
Step 2. (Images 2 and 3) Find out where it is exactly. You need to know what if any vital structures it may have pierced so you can plan for removal. In this stable patient, CT was the best option. If he had been unstable, it would have meant an immediate trip to the OR. Note how the object is within the chest wall, BUT it had penetrated at least as deep as the lung since a pneumothorax was present.
Step 3. (Image 4) Get it out! Off to the operating room for removal, just in case some unexpected bleeding or hemodynamic changes were to occur. After the patient was asleep, a chest tube was inserted. The object was a fine nail from a commercial nail gun mishap and pulled out easily with the hemostat. He was discharged two days later after the tube was pulled.
Photo source: personal archive. Patient not treated at Regions Hospital