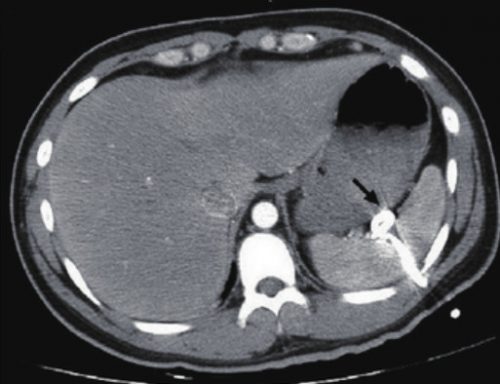
I previously described a trauma patient who had a pigtail type chest tube inserted with some odd CT findings after insertion:
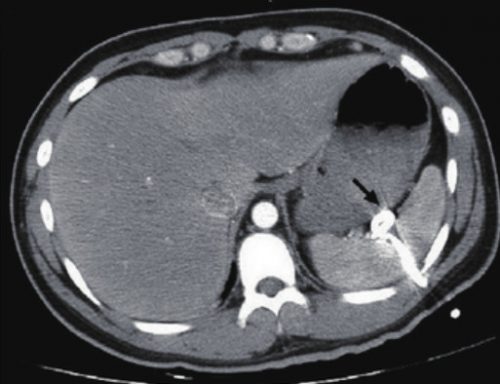
So what is wrong in this picture? Well, the catheter has been inserted into the spleen! This can occur if it is inserted too low, or if there are adhesions between lung and chest wall or diaphragm.
How can it be avoided? Make sure that the insertion point is no lower than the 5th intercostal space. This is the level of the nipple in a male. And depending on what type of kit you use, be careful! Some are based on Seldinger technique, which would seem to be a bit safer. Others use a small trochar, which can be inserted a little too deeply at times. Note that this complication can occur with any kit, and can also occur when using a standard tube and open insertion technique.
Does a pigtail tube even work for hemothorax? There’s some debate about this. Traumatic hemothorax is not defibrinated like a medical one. Thus, there are frequently clots present which may not fully evacuate through a standard chest tube, let alone a tiny one. Thus, I don’t recommend a pigtail for acute traumatic hemothorax.
How should I manage this issue? Obviously, this tube needs to come out. And assuming that the initial indication for the tube is still present, a better one needs to be inserted. Dont’ pull it out yet! First, look at the vital signs. If there is significant bleeding and/or vitals are not normal, an immediate trip to the operating room is in order. In this case, the patient will likely lose their spleen.
If vital signs are stable, book both an interventional radiology suite and an OR. Or better yet, use a hybrid room. Have the radiologist obtain a baseline angiogram, and position a catheter in the main splenic artery. Incrementally remove the pigtail, hand injecting a small amount of contrast each time. If extravasation is noted at any time, the radiologist can then attempt to embolize. If selective embolization isn’t successful, then the main splenic artery should be embolized. If embolization doesn’t work, or vital signs deteriorate at any time, the surgeon should immediately proceed to laparotomy. Attempts at splenic salvage will probably not be successful.
Finally, insert a new, conventional chest tube using finger guidance. Don’t make the same mistake twice! And by the way, this works for pigtails in the liver, too. They are less likely to bleed significantly when withdrawn, and obviously the radiologist can only used selective embolization if they do.