Today, I’m dusting off an old post on flying and diving after pneumothorax. This shows the thinking up until last year. Tomorrow, I’ll write about a new paper that suggests that we can shorten the “no-fly” time considerably.
Hint: no changes to the diving recommendations. One pneumothorax is likely to ground you forever.

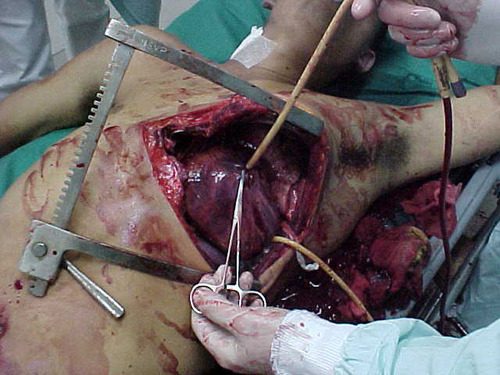
Patients who have sustained a traumatic pneumothorax occasionally ask how soon they can fly in an airplane or scuba dive after they are discharged. What’s the right answer?
The basic problem has to do with Boyle’s Law (remember that from high school?). The volume of a gas varies inversely with the barometric pressure. So the lower the pressure, the larger a volume of gas becomes. Most of us hang out pretty close to sea level, so this is not an issue. But for flyers or divers, it may be.
Flying
Helicopters typically fly only one to two thousand feet above the ground, so the air pressure is about the same as standing on the earth. However, flying in a commercial airliner is different. Even though the aircraft may cruise at 30,000+ feet, the inside of the cabin remains considerably lower though not at sea level. Typically, the cabin altitude goes up to about 8,000 to 9,000 feet. Using Boyle’s law, any volume of gas (say, a pneumothorax in your chest), will increase by about a third on a commercial flight.
The physiologic effect of this increase depends upon the patient. If they are young and fit, they may never know anything is happening. But if they are elderly and/or have a limited pulmonary reserve, it may compromise enough lung function to make them symptomatic. And having a medical problem in an aluminum tube at 30,000 feet is never good.
Commercial guidelines for travel after pneumothorax range from 2-6 weeks. The Aerospace Medical Association published guidelines that state that 2-3 weeks is acceptable. The Orlando Regional Medical Center reviewed the literature and devised a practice guideline that has a single Level 2 recommendation that commercial air travel is safe 2 weeks after resolution of the pneumothorax, and that a chest x-ray should be obtained immediately prior to travel to confirm resolution.
Diving
Diving would seem to be pretty safe, right? Any pneumothorax would just shrink while the diver was at depth, then re-expand to the original size when he or she surfaces, right?
Not so fast. You are forgetting why the pneumothorax was there in the first place. The lung was injured, most likely via tearing it, penetration by something sharp, or popping a bleb. If the injured area has not completely healed, then air may begin to escape through it again. And since the air used in scuba diving is delivered under pressure, this could result in a tension pneumothorax. This is disastrous underwater!
Most injuries leading to pneumothorax heal completely. However, if there are bone spicules stuck in the lung or more complicated parenchymal injuries from penetrating injury, they may never completely heal. This makes the diver susceptible to a tension pneumothorax anytime they use their regulator.
Bottom line: Most patients can safely travel on commercial aircraft 2 weeks after resolution of pneumothorax. Ideally, a chest xray should be obtained shortly before travel to confirm that it is gone. Helicopter travel is okay at any time, since they typically fly at 1,500 feet or less.
Divers should see a physician trained in dive medicine to evaluate their injury and imaging prior to making another dive.
Tomorrow: new info on flying after pneumothorax
References:
- Divers Alert Network – Pneumothorax – click to download
- Practice Guideline, Orlando Regional Medical Center. Air travel following traumatic pneumothorax. October 2009.
- Medical Guidelines for Airline Travel, 2nd edition. Aerospace Medical Association. Aviation, Space, and Environmental Medicine 74(5) Section II Supplement, May 2003.