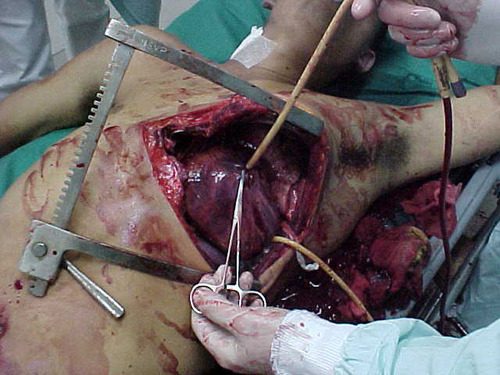
A few weeks ago, I opened a survey to find out common practices regarding performing emergency thoracotomy (EDT) in the emergency department. This procedure is performed at one time or another in most higher level trauma centers. It’s very invasive and is performed in an area that is not really set up for major operative cases. Furthermore, the atmosphere can be chaotic, and stress levels run high.
How safe is this situation? How does personal safety balance out with saving your patient? There are many, many opportunities for injury during this procedure, with significant exposure to blood and other bodily fluids.
A recently published multi-center study examined the potential for exposure during EDT at 16 US trauma centers over a 1.5 year period (14 Level I, 2 Level II). The study was prospective and observational, and was based on questionnaires filled out by all personnel involved in each procedure. A total of 1360 providers submitted information on 305 EDTs.
Here are the factoids:
- Mechanism was penetrating in 77% of patients, who were predominantly young and male (91%)
- 15 patients survived (5%), and 4 had residual neurologic impairment
- Only 56% of respondents wore full personal protective equipment (PPE)
- There was a 7% exposure rate per EDT(22 incidents), and 1.6% rate per participant in the case
- The majority of those exposed were trainees (68%) who were injured by something sharp (scalpel 39%, fracture 28%, needle 17%, scissors 3%)
- There was a strong correlation with PPE use and no exposure during the procedure
- Only 92% followed their hospital’s occupational exposure protocol if injured (!!!)
Bottom line: Emergency thoracotomy will always be a dangerous procedure. Things happen quickly, there is little time to properly prepare and sharp, pointy things are everywhere. But according to this paper, the actual exposure rate is low. Factoring in the risk of disease transmission, the risk to an individual provider of contracting HIV is 1 in a million, and for hepatitis C is 3 in 100,000.
The most distressing part of this study, to me, was the sense of invulnerability of a few of the participants. How can anyone justify not wearing full PPE during an emergency thoracotomy? I believe this represents a very casual attitude toward wearing PPE in any resuscitation. But this study clearly shows a large decrease in exposure rate when full PPEs are worn. Even more disturbing? The fact that 8% chose not to protect themselves by following their own institution’s occupational exposure protocol. Unforgivable!
The main takeaway messages are: always wear your PPE to a trauma resuscitation because you never know when you’ll need to get invasive (and won’t have time to dress up then), and be careful!!
Reference: Occupational exposure during emergency department thoracotomy: A prospective, multi-institution study. J Trauma 85(1):78-84, 2018.