Penetrating injuries of the lung come in two flavors: gunshot and stab. However, the end result for both is the same. They leak. And the leak is either air or blood. Having lower kinetic injury, stab wounds tend not to leak as much. Gunshots, on the other hand, can travel further through lung tissue and the higher energy causes more damage.
For the most part, managing these injuries is straightforward. The lung is essentially a sponge. Since most of it is air, the amount of damage done is much less than, say, to a solid organ. But bleeding and air leaks can be annoying in some cases, and even life-threatening in others.
Today, I’ll focus on injuries to the lung parenchyma. Here’s a basic primer on how to manage them.
- As always, the first decision to make is to answer the question, “do we need to go to the operating room right now?” This is always determined by unstable vital signs or symptoms that cannot be controlled with simple maneuvers like a chest tube.
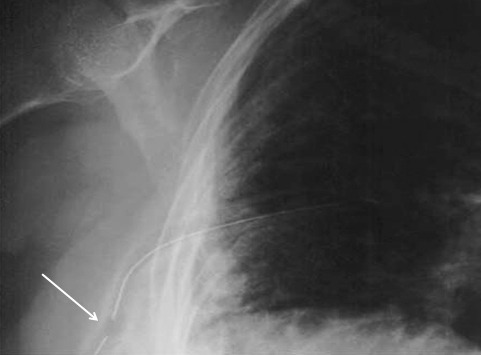
- Next, determine if any treatment is needed at all. The initial chest x-ray will tell you a lot.
- Is there any air or blood at all? If so, a followup chest x-ray after a set amount of hours (I use 6) will detect any progression that needs future treatment.
- Is there too much blood or air? If so, insert a chest tube.
- Is there too much ongoing air leak or bleeding? This indicates a problem (bronchial or chest wall / pulmonary vascular injury) that needs operative treatment.
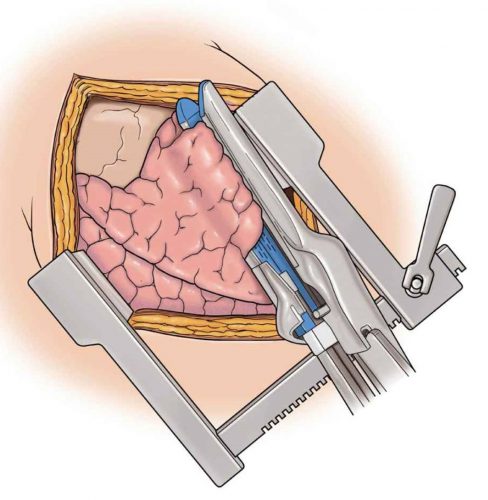
What are your options if you go to the operating room? Generally, an open thoracotomy is the most desirable, especially in the face of gunshots and major bleeding. It is fast and allows for rapid and complete exploration. VATS might be okay in a few stab wounds where the injury is thought to be limited but is still problematic.
Find the hole(s). With a single penetration, there are usually one or two holes. But there can be up to four if the wound traverses two lobes. And if is are more than one penetration, all bets are off.
Don’t poke a skunk. If a particular wound has no obvious bleeding or air bubbles, leave it alone. Save your efforts for the ones that are really a problem.
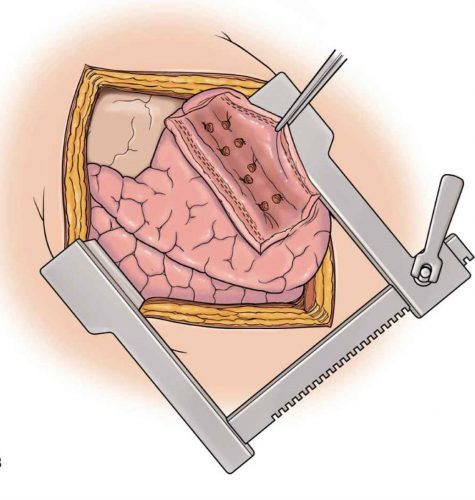
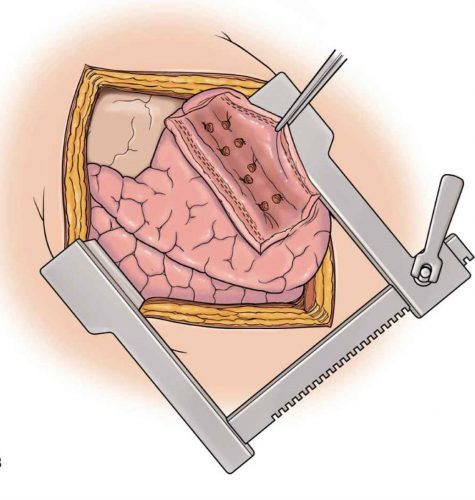
Use stapled tractotomy. Direct repair of lung wounds may lead to intra-parenchymal hematomas or air embolism. Wedge resection reduces lung volume, particular in patients with multiple injuries.
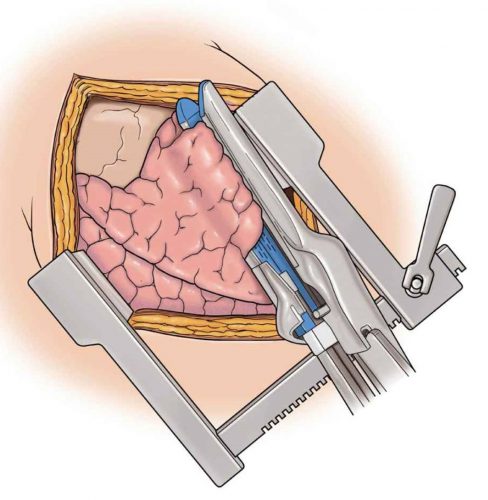
Here’s how to do it. Insert a GIA stapler through the bullet tract and fire. This will lay open the entire tract so that individual air leaks and bleeders can be individually suture ligated.
Then fully evacuate all blood from the chest and make sure there is no more bleeding. Failure to do so can result in retained hemothorax and the need for yet another operation. Insert a well-positioned chest tube to finish off the procedure.
Reference: Stapled pulmonary tractotomy: a rapid way to control hemorrhage in penetrating pulmonary injuries. JACS 185(5):467-487, 1997.