I’ve said it many times before: “don’t just read the abstract.” They can be misleading, and doing so makes it impossible to see the shortcomings of the research model and the veracity of the conclusions. Yet good trauma professionals do it all the time.
So I’ve selected a recent poster child to demonstrate this tenet. Let’s go over the study details:
This paper is a retrospective, registry review from Japan. The authors point out that one of the long-held rules is to avoid scanning unstable trauma patients in the “tunnel of death.” The authors cite a prior study that did not show an increase in mortality from this practice. So they decided to repeat/confirm it using 11 years of national registry data.
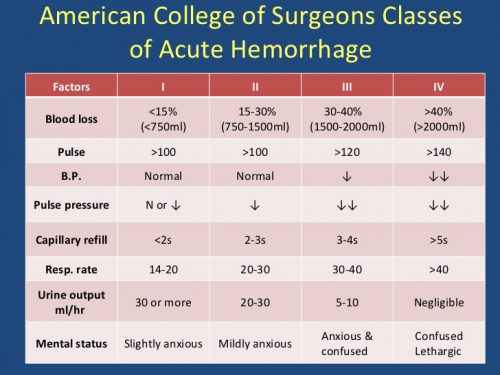
They included all patients who arrived at the trauma center with blood pressure < 90. Interestingly, they excluded patients in frank or near arrest. And finally, patients with critical data points missing were excluded. They used a regression method to control for covariates such as age, ISS, and vitals upon arrival.
Here are the factoids:
- Out of nearly 200,000 patients, about 7,000 were initially eligible. About 1,000 were excluded by the criteria above or because they were treated at a low volume facility. Only 5,809 were included in the study and another 500 were excluded because of missing covariates.
- The authors found that there were significantly fewer deaths in the group of unstable patients taken to CT (20 fewer per 100 patients) (!!!?)
- However, when corrected for confounders, this significant difference went away completely
- But the authors conclusion in the abstract was: “We suggest physicians should consider CT as one of the diagnostic options even when patients are unstable.”

Bottom line: What? The study went from showing that taking an unstable patient to CT was amazing for decreasing mortality, to no different after applying more statistical methods. And since there was no difference, why not just go?
Here’s why. In-hospital and 24 hour mortality are not good indicators of anything because there are so many patient and hospital factors involved. And because it was a registry study, there was no way of knowing if the patient was hypotensive at the time they were taken to CT. They could have had a low blood pressure and responded well to resuscitation. Or they could have been normotensive on arrival and became hypotensive before CT scan. There is no way to cleanly identify the correct study group without a prospective study, or a very painstaking retrospective one.
One of the most important aspects of this study is some background info that is not stated in the paper. Surgeon involvement in initial resuscitation in Japan is not nearly as integrated as it is in the US. So if the resuscitating physicians can’t do anything about the bleeding in the ED, why not just scan them while awaiting arrival of the surgeon? If the patient crashes, was it due to the scan, or a delay in getting to the OR?
So don’t just read the abstract. If it seems to be too good to be true, it is. Or at least self-serving. Read the nitty gritty details and decide for yourself!
Next week: more on unstable patients and the CT scanner
Reference: Computed tomography during initial management and mortality among hemodynamically unstable blunt trauma patients: a nationwide retrospective cohort study. Scand J Trauma 25(1):74, 2017.