How To Manage TBI In Patients On Warfarin
We all know that the combination of traumatic brain injury (TBI) and warfarin can be dangerous. Here at Regions, we developed a reversal protocol a few years ago. However, we found that just having a list of preferred “antidotes” to give was not enough. The time factor is very important, and we found that we needed to ensure prompt use of these medications when indicated.
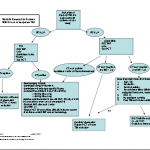
So we added features that ensured timely response and reversal. You can download the protocol by clicking the image above or the link at the bottom of this post.
First, we recognized that any patient with a known or suspected TBI who was taking warfarin was at risk. If the initial GCS was <14, then a full trauma team activation is called. This gives the patient priority lab processing and immediate access to the CT scan. In addition, 2 units of thawed plasma are administered while in the resuscitation room. If the head CT is negative, plasma is stopped.
For patients with a GCS of 14 or 15, a “Code RED” is called, ensuring that an ED physician sees the patient immediately. A point of care INR is drawn and the patient is sent for stat head CT. If the head CT is negative with INR>2.5, the patient is admitted for observation and a repeat head CT is obtained 12 hours later. We have seen patients develop delayed hemorrhage when they have high INR.
We apply a restrictive set of criteria to determine if a patient may go home from the ED, which causes us to admit most for observation. And if they do have a positive CT, we use the algoritm listed below for comprehensive management and reversal.
Bottom line: Patients with any head trauma and an elevated INR are a walking time bomb. They need prompt assessment and reversal of their anticoagulation if indicated. Feel free to share your protocols here as well by posting a comment.
Download the full protocol; click here.
Related post: