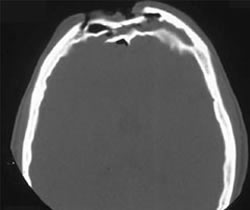
The tripod fracture (officially known as the zygomaticomaxillary complex fracture, and sometimes called a malar fracture) is the most common one seen after trauma. Fundamentally, the zygoma is separated from the rest of the face in a tripod fracture.
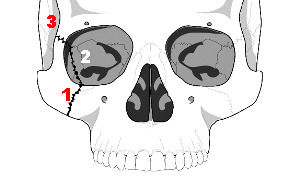
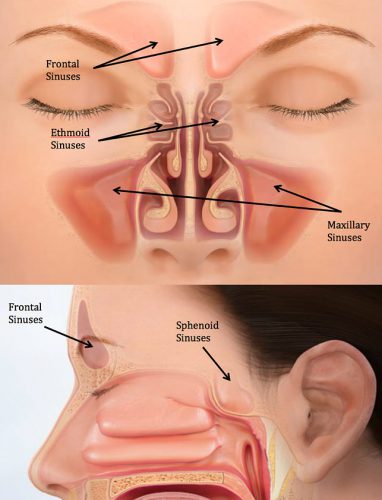
As you might imagine (tripod fracture), there are three components to this fracture. The first is a fracture through the zygomatic arch (1). Next, the fracture extends across the floor of the orbit and includes the maxillary sinus (2). Finally, the fracture includes the lateral orbital rim and wall (3).
Extraocular muscles may become trapped in the fracture line, leading to diplopia. It is very important to do a good eye exam to try to detect entrapment. The infraorbital nerve also passes through the orbital floor and may be injured, leading to numbness along the lower eyelid and upper lip.
Nondisplaced fractures are treated symptomatically and reevaluated after a week or so to see if surgery would be beneficial. Displaced or symptomatic fractures require early open reduction. The pictures below show the anatomy of these fractures. They are derived from teaching materials provided by the Radiology Department at the University of Washington.