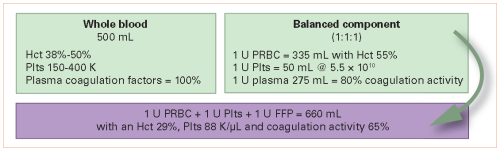
Decades ago, blood banks discovered they could fractionate units of whole blood into components for focused use. This was useful for patients who were thrombocytopenic or needed specific plasma factors. But trauma patients bleed whole blood, and trying to reassemble whole blood from components does not work well. Have a look at this chart:
It all comes down to money. Blood banks found they could charge more for the sum of the components of a unit of whole blood rather than the one unit itself. But now, with whole blood in trauma becoming a thing again, it’s essential to reexamine costs.
The University of Texas at San Antonio group examined transfusion-related charges for trauma patients receiving either component therapy or low-titer O+ whole blood within six hours of arrival. This was a retrospective review of prospectively collected data. During the first two years, only component therapy was given. Whole blood was introduced during the last four years.
Here are the factoids:
- Once the trauma center switched to whole blood, total annual transfusion charges, as well as component charges decreased by 17% overall
- In both adults and children, whole blood was associated with a significantly lower cost per ml delivered and cost per patient throughout all phases of care
- In severely injured patients (ISS>15), the same significantly lower costs were also noted
- Patients who triggered the massive transfusion protocol also had a lower cost per ml of product in the ED and the first 24 hours
The authors concluded that whole blood was associated with lower charges and “improved logistics,” especially in massive transfusion patients.
Bottom line: This is an interesting and important paper. However, several questions still need to be answered. I recognize that there is limited space in an abstract, so I will list them below in hopes the authors will answer them during the presentation.
The first issue is that the numbers of patients and quantities of blood products given need to be listed. These are very important because the figures list only total charges and maybe costs. These numbers are not per unit of product, so the data may be skewed if the number of patients was different between the groups. For example, if 100 patients received component therapy and only 10 got whole blood, costs or charges could definitely be skewed.
And then there is the cost vs. charge confusion. The abstract seems to use them interchangeably. The methods section of the abstract states that charges were analyzed. Yet cost is mentioned in the results, and figure two shows “cost” on the axes, but the caption states that charges were listed.
We all know that hospitals can charge whatever they like, and that amount may vary based on insurance and other factors. The relationship between the charge and the cost is tenuous at best. Hopefully, the authors will clarify this at the start of the presentation.
Here are my comments and questions for the presenter/authors:
- Please clarify the concept of charges vs. costs at the presentation’s beginning. If you truly analyzed only charges, do they bear any relationship to the actual costs of the units?
- Shouldn’t your analysis of annual “charges” for product expenditures in Figure 1 be per unit? Otherwise, the costs and charges could be lower if fewer products were given after whole blood was introduced.
- Was the switch to whole blood absolute, or was component therapy still given in some cases after 2018? If the switch was not total, there could be a selection bias in patients who received whole blood.
- Figure 2 also appears to be total charges (or costs), not per patient or unit. But, again, without numbers it is difficult to say if the dollar differences are significant.
- What are the “improved logistics” mentioned in the conclusion section? And how could they lower charges (or costs) in your study?
Lots of questions. I think you will need to provide a lot of explanation up front to justify your findings. Nevertheless, I’m excited about the presentation.
Reference: TRANSFUSION-RELATED COST COMPARISON OF TRAUMA PATIENTS RECEIVING WHOLE BLOOD VERSUS COMPONENT THERAPY. EAST 2023 podium abstract #28.
