In my last post, I noted that nonoperative management is the norm for dealing with high grade renal injuries. One of the possible options, angioembolization, was relatively infrequently used at only 6% of the time.
For management of other organs like the spleen, there are several angioembolization options. Depending on the type and severity of injury, selective (partial) or nonselective (main splenic artery) embolization can be carried out. For the liver, only selective embolization can be used. But what about the kidney?
Are there consequences of nonselective renal embolization? Or should we always strive for selective control? The urology group of the University of Tennessee – Knoxville published a series of papers on their experience using embolization in patients with the most severe injuries (Grade 5). They retrospectively examined just over 3 years of admissions with this injury. Numbers were very small (6 men, 3 women).
But they also published a second paper, extending the review dates to capture one more male patient. And they followed this group for 1.5 to 5 years (mean 2.5 years) to determine if any delayed complications surfaced.
Here are the factoids:
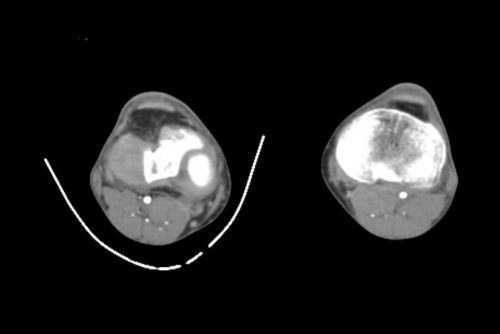
- Seven patients underwent full, nonselective embolization, and the other three had “super selective” embolization
- All patients had control of bleeding without surgical intervention
- Followup CT imaging showed no persistent extravasation or expanding hematoma
- No patient developed complications, such as a retroperitoneal abscess, prolonged fever, or hypertension while in the hospital or during short-term followup
- Most patients showed a very small increase in serum creatinine (mean 0.04), but one patient increased from 1.1 to 1.7
- On longer term followup, one patient, age 51, developed hypertension 10 months after his injury. It is not possible to determine whether he was one of the 20% of older adults who develop hypertension, or whether it was due to the procedure. it was well-controlled with a single antihypertensive med.
- None developed altered renal function, stones, chronic pain, fistula, or pseudoaneurysm
Bottom line: Obviously, the data is very limited with only 10 patients. However, it is very interesting to note that the majority of these patients underwent nonselective embolization of the renal artery without any adverse event. The one case of hypertension occurred with nonselective embolization, although I have seen several case reports where this occurs with selective embolization as well.
It is now well-accepted that high-grade renal injury can and should be managed nonoperatively if the patient’s hemodynamic status is reasonable. I recommend a trip to interventional radiology if the patient has active extravasation or a high-grade (Grade 4 or 5) injury, as these patients are at risk for loss of the entire kidney otherwise. Selective embolization can be attempted first, but don’t be shy to take out the entire organ if need be.
References:
- Percutaneous embolization for the management of Grade 5 renal trauma in hemodynamically unstable patients: initial experience. J Urology 181:1737-1741, 2008.
- Intermediate-term follow-up of patients treated with percutaneous embolization for Grade 5 blunt renal trauma. J Trauma 69(2):468-470, 2010.