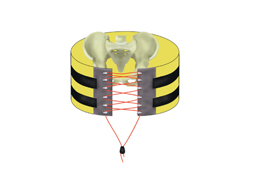
Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) is one of the newer shiny toys that trauma professionals have adopted over the past 8 years or so. It is used to buy time for a patient who is near arrest in order to temporarily stop bleeding and get them to the operating room.
And as with all new toys, everyone wants one! I have always advised caution. Adopt a data-based approach to toy usage. Unfortunately information has been accumulating ever so slowly on this one. To help remedy this, the AAST created a registry in 2013 to consolidate the low REBOA experience numbers accruing across the US.
A group of seven surgeons representing higher-volume REBOA centers collaborated to review the AAST AORTA registry, which prospectively collects data on patients who undergo aortic occlusion. They retrospectively reviewed over six years of data on adult patients receiving REBOA for pelvic injury. They examined demographic, procedural, and outcome data in patients who underwent this procedure, both with and without other interventions like preperitoneal packing, angioembolization, or external fixation. For inclusion in the study, patients needed to have sustained blunt trauma and survived beyond the emergency department.
Here are the factoids:
- Of the 207 patients with pelvic (Zone 3) REBOA in the registry, only 160 met inclusion criteria
- Patients who only had REBOA suffered a mortality rate of 40% (5% in OR and 35% in the ICU)
- Patients who had REBOA plus one of the other interventions had a 31% mortality rate (6% in OR and 25% in ICU)
- Patients who had REBOA plus two other interventions also had a 31% mortality rate (12% in OR and 30% in the ICU)
- Adding external fixation with or without another adjunct appeared to decrease mortality by half (from 50% to about 25%)
- Complications were very common in all subsets, ranging from 35% to 86%
- Patients receiving more interventions typically were more severely injured
- No combination of REBOA and adjuncts was superior, but addition of an external fixator did appear to improve survival
- Patients receiving angiographic embolization had a higher incidence of AKI, sometimes resulting in the need for dialysis
- There were no significant outcome differences with REBOA use alone or with additional adjuncts
Bottom line: This was a primarily a descriptive study of how REBOA is integrated into pelvic fracture care at select US trauma centers. It was not really designed to compare the efficacy of REBOA vs preperitoneal packing vs angioembolization vs external fixation of the pelvis.
But it does show that survival remains dismal in these patients and the complication rates of REBOA + adjunct use are considerable. The authors correctly conclude that REBOA is being used in the treatment of pelvic fractures, frequently with the addition of other adjuncts. They state that the benefit of more interventions must be balanced against the potential for complications. And finally, they note that there is a need to fill in the evidence base if we are ever to adopt REBOA as a standard of care for select pelvic fractures.
What does this mean to all of you who are thinking of playing with this toy? Proceed with caution! The learning curve is steep. The complication rate is high. The opportunity for mayhem is great. This means that you must proceed deliberately. Get some advanced training with this technique. Use your performance improvement program to impartially critique its use with every deployment. And submit your experience to the national registry so we can all learn from your experience and figure out how to optimize use of this tool.
Reference: Patterns and outcomes of zone 3 REBOA use in the management of severe pelvic fractures: Results from the AAST Aortic Occlusion for Resuscitation in Trauma and Acute Care Surgery database. J Trauma 90(4):659-665, 2021.