I’m just getting back from a speaking engagement at the 30th Annual (!) Parkview Trauma Symposium in Fort Wayne, Indiana. I love traveling around the country and speaking, because I have the opportunity to hear other fascinating speakers and pick up new tidbits for personal use and to share. This was one of my favorite symposia and the speakers were fantastic.
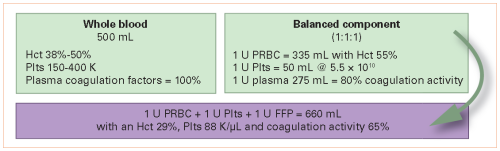
My colleague, Scott Thomas, is the Trauma Medical Director at Memorial Hospital of South Bend in Illinois and gave an excellent talk on goal directed, whole blood transfusion. The use of whole blood is growing in the US, as I’ve written about previously. However, I was totally unaware of the systematic use of this product in a unique industry: cruising.
Royal Caribbean Cruise Lines (RCCL) implemented a whole blood transfusion program in 2008 on a subset of its more than 40 cruise ships. The guests on cruise ships tend to be an older population, similar to what many trauma centers in the US encounter. Similarly, many have medical comorbidities that require them to take anticoagulants or antiplatelet agents, and they may develop bleeding conditions while on board.
A good deal of cruise time is spent at sea and away from ports that have major medical facilities. Helicopter transport from the ship is not readily available due to distance from shore, so patients who experience serious illness must be cared for in the onboard medical facilities until within striking range of a faster coast guard ship. It is not practical to store blood on board, so bleeding patients presented a real problem in the past.
In response to this, RCCL implemented a program that was very forward thinking for its time. It emphasized:
- Transfusion based on hemodynamics, not a hemoglobin reading
- Anticoagulant reversal, if possible
- Use of TXA
- Limited use of crystalloid
- Permissive hypotension
- Use of fresh, whole blood
Wow! And this was 10 years ago. In my next post, I’ll start working through the protocols and logistics that RCCL uses for this program in the (relatively) austere medical / trauma environment aboard a cruise ship.
Related post: