This is an uncommon injury. But when encountered it can cause the trauma professional (and the patient) some major headaches. The majority of the vertebral artery injuries you are likely to encounter are caused by blunt trauma. They are generally diagnosed using CT angiography, and the treatment usually consists of low dose anti-platelet agents like aspirin. Occasionally, coiling or stenting using interventional radiology is needed.
But penetrating trauma is a totally different animal. Gunshot is the most common mechanism, because of the small windows available to access the artery within the vertebral canal using a knife. See the course of the artery in the picture below:
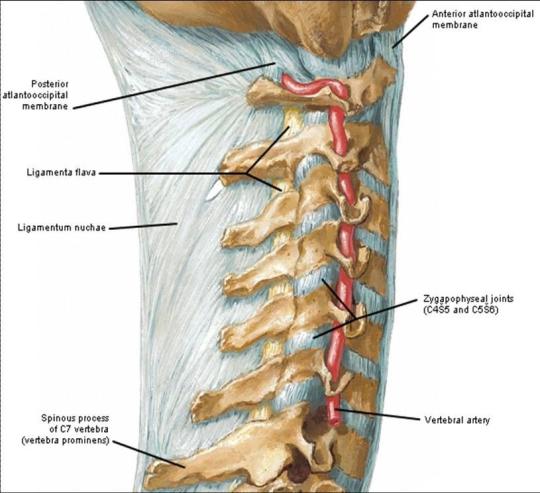
Unfortunately, this bony cage also makes it difficult to surgically approach the artery, especially if the field is continually filling with blood.
The techniques for dealing with this injury according to the doctor books are:
- Send the patient to interventional radiology. Cutting off flow using coils is the preferred technique. Gelfoam and other products are not used because of the concern for distal embolization (to the brain). Stenting may be a consideration for blunt trauma, but not for penetrating.
- Or, obtain proximal control by ligating the vertebral artery as it takes off from the subclavian. Hmm, this requires either a separate incision, or a supraclavicular extension of your neck incision. It takes time and is not as easy as it sounds.
Generally, the trauma surgeon stumbles upon this injury while doing a trauma neck exploration. Bleeding can be pesky, and may serve to obscure the field. My preferred method of control is:
- Jam a wad of bone wax into the vertebral canal right where the bleeding is coming from.
- Then jam another wad into the canal in the space below it. Proximal control!
- Jam one final wad into the space above, if accessible. Distal control!
End of problem. Then do a thorough evaluation for all other injuries and address them. Feel free to share any additional tips that you may have!
