I’ve been discussing the Glasgow Coma Scale (GCS), but only the adult version so far. The pediatric GCS was created about 10 years after the classic adult scale after it was recognized that several of the scores were not appropriate for younger non-verbal children, typically less than one year of age. It has been validated several times over the ensuing years and has been integrated into our trauma practices.
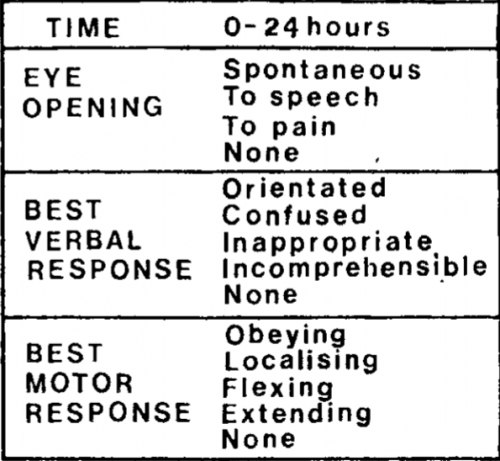
So what is different about the pediatric GCS scale? It has the same three main components, eye opening, best verbal response, and best motor response. The number of scores under each remains the same as well. The major changes occurred in the verbal response scores. Here’s the breakdown; I’ve highlighted the differences.
Eye Opening
- All components are the same as for adults
Best Verbal Response
- No response to stimuli
- Inconsolable, agitated
- Inconsistently inconsolable, moaning
- Cries but consolable. Has appropriate interactions.
- The child smiles, orients to sounds, follows objects, and interacts with adults
Best Motor Response
- No response to stimuli
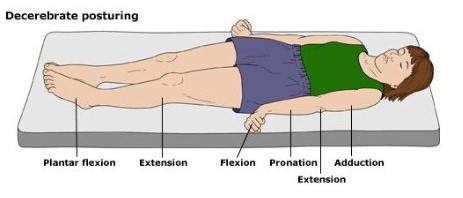
- Decerebrate posturing (extension to stimulation, see the adult post for details)
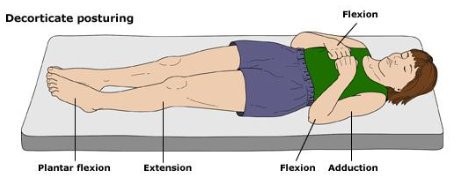
- Decorticate posturing (flexion to stimulation, see the adult post for details)
- Withdraws from pain
- Withdraws from touch
- Spontaneous, purposeful movement
In my next post in the series, I’ll review what’s new with the GCS-40 score.
Reference: Neurologic evaluation and support in the child with an acute brain insult. Pediatric Annals 15(1):16-22, 1986.