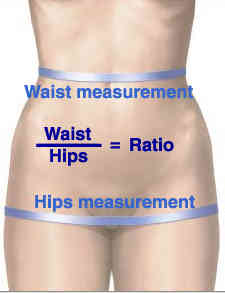
Yesterday, I wrote about a study that looked at a CT scan-derived index that promised to predict complications and mortality based on the waist-hip ratio. It was actually a very good one. But there is another abstract being presented at the American College of Surgeons Clinical Congress this week that promises miracles from the CT scanner as well.
This next abstract looks at muscle mass in trauma patients, as measured by CT scan. Specifically, the authors measured the density of the psoas muscle by determining its cross-sectional area and its density in Hounsfeld units. They then looked at the relationship between this and 90 day mortality, complications, and disposition location.
Really? Well, here are the factoids:
- The study involved only 152 patients age 45+ from the year 2008
- Median ISS was only 9
- Patients with the lowest psoas cross-sectional area had an associated significantly higher death rate
- Those with lowest psoas density had an associated increase in complications, dependency on discharge, and mortality
- The authors suggest that these measurements could aid in patients who would benefit from aggressive nutritional support and physical therapy, and could aid in discharge planning
Bottom line: Very different from yesterday’s abstract. This one has no grounding in prior research. It appears to be one that was just dreamed up from nowhere. And it is truly an association study. No causality can or should be inferred.
There were only 152 patients studied. From 2008. Why? Why didn’t the authors use a more contemporary dataset? There is something weird going on behind the scenes. Is this an old study that was forgotten, and is just now being conveniently dusted off for analysis and submission? A power analysis to find out how many patients should be reviewed is not possible, so it is important to err on the high side. Not just 152 patients.
If you were to just read the abstract and especially the conclusions, you really might get the wrong idea. This is a study that will not see it’s day in any journal. Read and learn from it. But don’t duplicate it!
Related post:
Reference: Computed tomography-measured psoas density predicts complications, discharge location, and mortality in trauma patients. ACS Scientific Forum, trauma abstracts, 2016.