How To Remove A Chest Tube
Tag Archives: chest tube
How To Predict the Need for Chest Tube in Occult Pneumothorax
Occult pneumothorax occurs somewhere between 2% and 12% in all blunt trauma patients. Many of these pneumothoraces never progress and thus never need treatment. Is there a way that we can identify ones that are likely to get worse?
A retrospective study of 283 blunt trauma patients with occult pneumothorax was presented at the EAST Annual Scientific Assembly last January. A total of 98 of these patients underwent chest tube insertion within 7 days, and 185 patients were successfully observed.
The authors noted an inverse relationship between age and successful conservative management. Patients with more serious injuries failed expectant management more frequently. Finally, patients with more rib fractures also tended to fail.
The authors estimated the risk of failure of expectant management based on these critieria and found:
- Age > 35 – 36%
- ISS > 24 – 20%
- Rib fractures >= 4 – 53%
The risk with having none of these was 10%, and the risk with all was 75%!
The time interval for placement was also interesting. 80% of the failures requiring a chest tube occurred within 24 hours, with most occurring in the first 2 hours. The authors also found that 40% of patients who were placed on a ventilator failed.
Obviously, this is a small retrospective study and the exact criteria for placing a chest tube were not specified. Nevertheless, it provides a simple tool that allows us to keep an eye on a subset of patients who are likely to fail observation of occult pneumothorax.
Reference: Factors Predicting Failed Observation of Occult Pneumothoraces in Blunt Trauma. Selander, Med Univ of South Carolina. EAST 2010 Annual Scientific Assembly.
How To: Chest Tube Insertion For Trauma
Here’s a short video that shows you everything you need to know. Enjoy!
Chest Tubes and Autotransfusion
Chest trauma is common in trauma patients. Chest tubes are required with some regularity for the management of hemothorax and/or pneumothorax. Occasionally, the amount of blood in the chest is substantial, and when the tube goes in we wish that we were able to transfuse that blood.
Well, you can! Most collection systems have optional autotransfusion canisters that connect to the chest tube inline with the collection system. The canisters are used to collect shed blood and can then be hung like a bag of blood from the blood bank.
A few key points about using autotransfusion canisters:
- I recommend you consider it for any chest tube being inserted for trauma. They will almost always have some blood in their chest.
- If you want to limit use further due to the expense, just add it for trauma activation patients.
- Always add it to the chest tube collection system before the chest tube goes in. Most of the blood will be lost if the chest tube is hooked to the collection system first.
- No need to anticoagulate the blood. Most systems can be used to reinfuse shed blood up to 6 hours after collection without heparin or other products.
- Be sure to use an inline blood filter. There will be some debris and clumps that must be removed.
- Don’t use the blood if it is likely to be contaminated. This most often occurs with penetrating trauma, where a stab or gunshot could injure stomach or colon and violate the diaphragm.
- Follow the manufacturer’s instructions for your brand of collection system.
Here’s a picture of an autotransfuser that attaches to a Pleur-Evac brand system.

The Right Way to Treat Tension Pneumothorax
Tension pneumothorax is an uncommon but potentially lethal manifestation of chest injury. An injury to the lung occurs that creates a one-way valve effect, allowing a small amount of air to escape with every breath. Eventually the volume becomes so large as to cause the lung and mediastinum to push toward the other side, with profound hypotension and cardiovascular collapse.
The classic clinical findings are:
- Hypotension
- Decreased or absent breath sounds on the affected side
- Hyperresonance to percussion
- Shift of the trachea away from the affected side
- Distended neck veins
You should never diagnose a tension pneumothorax with a chest xray or CT scan, because the diagnosis is a clinical one and the patient may die while these procedures are carried out. Having said that, here’s one:

The arrow points to the completely collapsed lung. Note the trachea bowing to the right.
As soon as the diagnosis is made, the right thing to do is to “needle the chest.” A large bore angiocath should be placed in the second intercostal space, mid-clavicular line, sliding right over the top of the third rib. The needle should then be removed, leaving the catheter.
The traditional large bore needle is 14 gauge, but they tend to be short and flimsy. They may not penetrate the pleura in an obese patient, and will probably kink off rapidly. Order the largest, longest angiocath possible and stock them in your trauma resuscitation rooms.
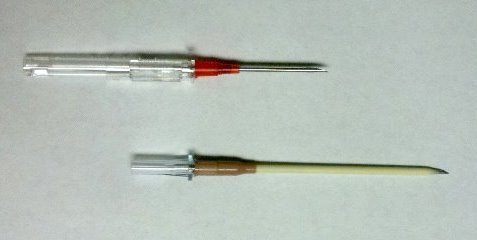
The top catheter in this photo is a 14 gauge 1.25 inch model. The bottom (preferred at Regions) is a 10 gauge 3 inch unit. Big difference! And if the patient is extremely obese, make a 1 cm cut in the skin and sink the hub deep to the skin for extra distance.
The final tip to treating a tension pneumothorax is that a chest tube must be placed immediately after inserting the needle. If the patient is on a ventilator, the positive pressure will slowly expand the lung. But if they are breathing spontaneously, the needle will change the tension pneumothorax into a simple open pneumothorax. Patients with other cardiovascular problems will not tolerate this for long and may need to be intubated if you dawdle.

