Chest tubes are needed occasionally to help manage chest injuries. How do you decide when they are ready for removal?
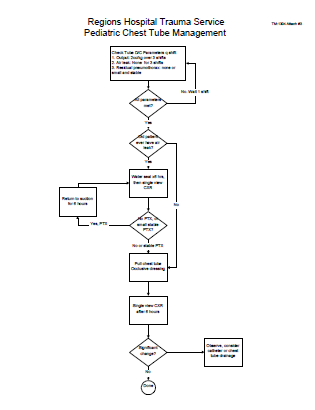
Unfortunately, the literature is not very helpful in answering this question. To come up with a uniform way of pulling them, our group looked at any existing literature and then filled in the blanks, negotiating criteria that we could all live with. We came up with the following. Click the image to see a full-size version, or click the link below.
Removal criteria:
- No (or a minimal, stable) residual pneumothorax
- No air leak
- Less than 150cc drainage over the past 3 shifts. We do not use daily numbers, as it may delay the removal sequence. We have moved away from the “only pull tubes on the day shift” mentality. Once the criteria are met, we begin the removal sequence, even in the evening or at night.
Removal sequence:
- Has the patient ever had an air leak? If so, they are placed on water seal for 6 hours and a followup AP or PA view chest x-ray is obtained. If no pneumothorax is seen, proceed to the next step. If there was no air leak, skip this step.
- Pull the tube. Click here to see a video demonstrating the proper technique.
- Obtain a followup AP or PA view chest x-ray in 6 hours.
- If no recurrent pneumothorax, send the patient home! (if appropriate)