Yesterday I posted an image of an unusual chest CT. The patient had been involved in a motorcycle crash weeks ago, and presented with new onset chest pain and weakness.
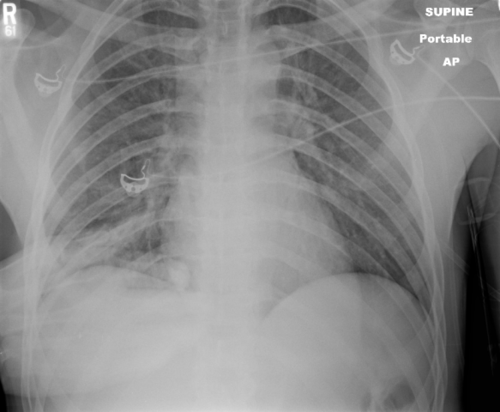
Exam of the chest showed a hint of diffuse swelling on the left side and moderate tenderness. Chest x-ray suggested a mild effusion on the left. I showed one slide of the CT yesterday, which showed a large amount of complex material in the chest wall. This is most likely a mixture of blood and clot.
Here is another slice of the CT that is more revealing:

Now you can see that there are multiple rib fractures present. While comparing the original and the recent scan, it is apparent that the fractures are more displaced on the recent one. Upon closer questioning the patient admits that he did fall down the day before the new pain and swelling occurred.
And by the way, he forgot to mention the fact that he had developed deep venous thrombosis and was taking warfarin! And also by the way, his blood pressures were becoming a bit soft.
I would consider this life-threatening bleeding! Crystalloid and blood resuscitate immediately. Reverse the anticoaguation quickly, using prothrombin complex concentrate (PCC, preferably 4-factor). Then send him to interventional radiology to see if there are any active bleeders that can be embolized. Finally, it’s off to the ICU to finish up the resuscitation and restore him to normal!
Related posts: