Hemostatic resuscitation (HR) is the new buzzword (buzz phrase?) these days. The new ATLS course touts it as a big change, and quite a few publications are being written about it. But, like many new things (think Factor VII), will it stand the test of time?
It has long been recognized that hemorrhage from trauma is bad. Mortality rates are high, and traditional management with crystalloids and then blood products leads to persistent coagulopathy, troublesome bleeding, tissue injury, and finally death. HR was devised to address the early coagulopathy. It concentrates on early coag correction with plasma and platelets, permissive hypotension, and rapid definitive correction of hemorrhage.
The end result of HR has been measured, and both organ perfusion and coagulopathy can be corrected with it. Unfortunately, these measurements are typically taken once hemorrhage control has been achieved. Is looking at (or beyond) the endpoint really the best way to gauge its effectiveness?
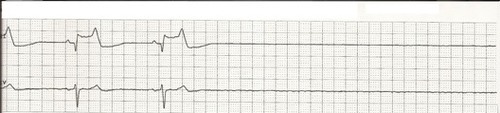
A robust multicenter study scrutinized looked at coagulopathy correction and organ perfusion during active hemostatic resuscitation. They used ROTEM to gauge the former, and lactate levels for the latter. Values were measured on arrival and after administration of every 4 units of blood. Only patients who received at least 4 units were included (106 subjects).
Here are the factoids:
- Average admission lactate was 6.2 meq/L, so these patients were sick
- Patients with a lactate > 5 did not clear it until after hemorrhage was controlled and no further blood was needed
- 43% of patients were coagulopathic by ROTEM on arrival.
- Coagulopathy increased for every 4 units of blood given, despite a plasma infusion ratio of close to 1:1 throughout their resuscitation
Bottom line: This was a well-done study on a relatively large number of patients, although a number of weaknesses and potential improvements are pointed out in the discussion. There’s a lot of data in the paper, and I urge you to read it in depth. But it seems to show that hemostatic resuscitation is not necessarily doing what we want it to do during the acute phase of hemorrhage. Both bleeding AND transfusions must be stopped before it appears to work. And even then, there is a delay before ROTEM and lactate parameters return to normal. For now, rapid control of hemorrhage is of utmost importance. We still need to figure out how tools like ROTEM or TEG and various serum markers will help us while we accomplish it.
Reference: Hemostatic resuscitation is neither hemostatic nor resuscitative in trauma hemorrhage. J Trauma 76(3):561-568, 2014.