In the US, Level I and II trauma centers are required to have around the clock neurosurgical coverage. This becomes problematic, especially in more rural areas, because they are a scarce resource. This problem is not limited to the States, and other countries have learned how to deal with it in their own ways.
A recent paper from Austria and the Slovak Republic looked at how this issue is dealt with at some centers in central Europe, and the impact of having neurosurgical procedures performed by trauma surgeons. The researchers looked at various databases maintained by 10 tertiary care hospitals in a retrospective fashion. Patients were included if they had a GCS of 8 or less and they survived to ICU admission. Some centers had neurosurgeons available, while others had only trauma surgeons. Procedures were performed by the appropriate type of surgeon in each center.
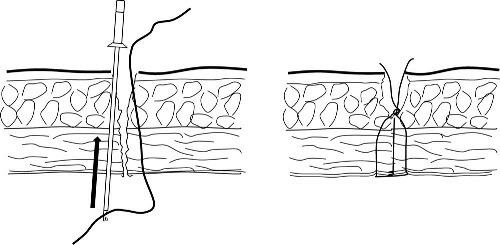
A total of 743 patients were evaluated, and about 68% underwent a neurosurgical procedure while 6% had an ICP monitor inserted. About a quarter of these patients had other significant associated injuries and were excluded, since the authors were interested in measuring effects in TBI patients. This left 311 patients, of whom 61% were treated by neurosurgeons and the remainder by trauma surgeons.
Here are some of the interesting findings:
- Prehospital airway was provided more frequently in the neurosurgical treatment group, which should potentially improve outcome
- ED management time and time to OR was shorter in the neurosurgical treatment group, which should also potentially improve outcome
- However, there was no difference in ICU survival, hospital survival, or long-term outcome!
Bottom line: This is an interesting but poorly constructed study. Don’t believe the results! Other researchers’ leftover databases were used, and some databases were excluded because “quality of care was not comparable” to other centers. This is the worst kind of selection bias! If you believe the results, then you would also have to believe that airway control and prompt operative management don’t really matter much. The paucity of neurosurgeons who are interested in trauma care is pervasive. However, we still need to look for solutions to this problem and they remain a very valuable member of the trauma team.
Reference: Outcome of patients with severe brain trauma who were treated either by neurosurgeons or by trauma surgeons. J Trauma 72(5):1263-1270, 2012.