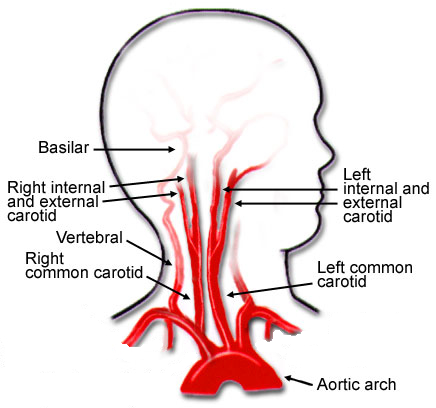
Blunt carotid and vertebral artery injuries (BCVI) are an under-appreciated problem after blunt trauma. Several screening tools have been published over the years, but they tend to be unevenly applied at individual trauma centers. I will discuss them in detail in the next section.
For the longest time, the overall incidence of BCVI was thought to be low, on the order of 1-2%. This is the number I learned years ago, and it has not really changed over time.
But how do we know for sure? Well, the group at Birmingham retrospectively reviewed every CT angiogram (CTA) of the neck they did in a recent two-year period. They did this after adopting a policy of imaging each and every one of their major blunt trauma patients for BCVI. Each patient chart was also evaluated to see if the patient met any of the criteria for the three commonly used screening systems.
During the study period, a total of 6,287 of 6,800 blunt trauma patients underwent BCVI screening with CTA of the neck. They discovered that 480 patients (7.6%) were positive for BCVI!
This is a shocking 8x higher than we expected! Why hasn’t this been obvious until now? Most likely because we were previously only aware of patients who became symptomatic. Luckily, many of these patients dodge the proverbial bullet and never exhibit any symptoms at all.
So why should we be worried? This is one of those clinical entities like blunt thoracic aortic disruption that potentially has terrible consequences if ignored. Although the number of patients who develop sequelae from their BCVI is small, suffering a stroke can be catastrophic.
Should we perform a screening study for all blunt trauma patients? Seems like overkill, or is it? Is there any way we be more selective about it?
In the next post, I’ll review the three current screening tools used to determine which patients should receive CTA, and how good they are.
Reference: Universal screening for blunt cerebrovascular injury. J Trauma 90(2):224-231, 2021.