Current events are making this classic post even more poignant!
The VIP syndrome occurs in healthcare when a celebrity or other well-connected “important” person receives a level of care that the average person does not. This situation was first documented in a paper published in the 1960s which noted that VIP patients have worse outcomes.
Who is a VIP? It may be a celebrity. A family member. Or even a colleague. Or the President of the United States. VIPs (or their healthcare providers) may have the expectation that they can get special access to care and that the care will be of higher quality than that provided to others. Healthcare providers often grant this extra access, in the form of returned phone calls and preferential access to their clinic or office. The provider tries to provide a higher quality of care by ordering additional tests and involving more consultants. This idea ignores the fact that we already provide the best care we know how, and money or fame can’t buy any better.
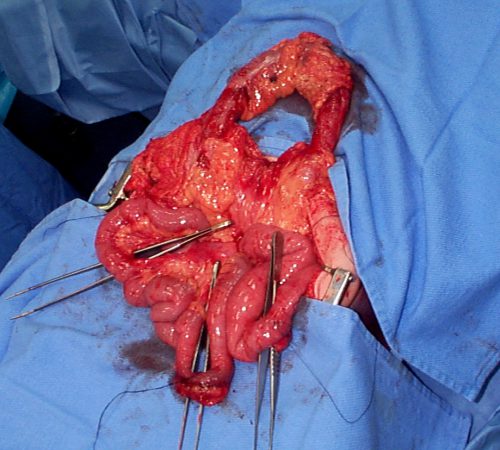
Unfortunately, trying to provide better care sets up the VIP for a higher complication rate and a greater chance of death. Healthcare consists of a number of intertwined systems that, in general, have found their most efficient processes and lowest complication rates. Any disturbance in this equilibrium of tests, consultants, or nursing care moves this equilibrium away from its safety point.
Every test has its own set of possible complications. Each consultant feels compelled to add something to the evaluation, which usually means even more tests, and more possible complications. And once too many consultants are involved, there is no “captain of the ship” and care can become fragmented and even more inefficient and dangerous.
How do we avoid the VIP Syndrome? First, explain these facts to the VIP, making sure to impress upon them that requesting or receiving care that is “different” may be dangerous to their health. Explain the same things to allproviders who will be involved in their care. Finally, do not stray from the way you “normally” do things. Order the same tests you usually would, use the same consultants, and take control of all of their recommendations, trying to do things in your usual way. This will provide the VIP with the best care possible, which is actually the same as what everybody else gets.
Reference: “The VIP Syndrome”: A Clinical Study in Hospital Psychiatry. Weintraub, Journal of Mental and Nervious Disease, 138(2): 181-193, 1964.