Delayed or missed diagnoses happen. It’s a reflection on the state of technology and our own diagnostic acumen. Unfortunately, a few cases of delayed diagnosis result in morbidity, potential lawsuits, and rarely, death.
How often does delayed diagnosis occur? A few spot check type articles were published about 15 years ago, but little has been done to slice and dice the data. And as usual, the old data ranged widely in its assessment of the incidence of this problem (1-18% !). However, I managed to find a (somewhat) more recent one that gives a little clearer picture of this issue.
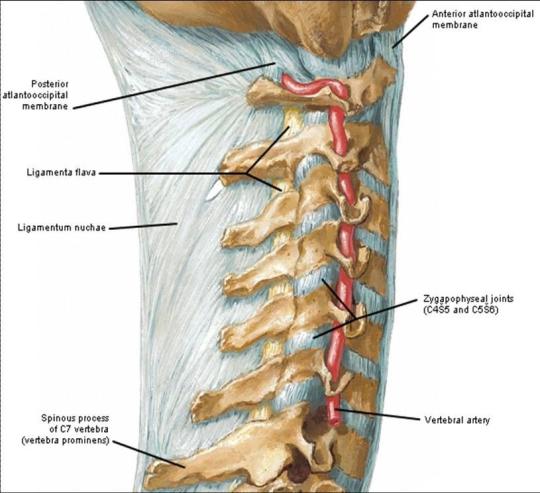
A single pediatric hospital in Indiana reported its experience from 1997 to 2006. This interval included the time that it was verified as a Level II Trauma Center (2000 onwards). They included children 0-14 who had sustained “major trauma.” This was defined as multiple system injuries, high-energy impacts, and gunshots. In this study, delayed diagnosis was defined as one found after a stable patient was admitted to their room. In patients taken directly to OR, it was one found after the patient left the recovery room.
Here are the factoids:
- 1100 patients met study criteria. 98% were blunt trauma.
- Only 44 patients had delayed diagnoses of 47 injuries
- Average time to diagnosis was 4 days (range 8 hours to 28 days)
- 34% of diagnoses were made within 24 hours
- 3 diagnoses were made at a followup visit, all for upper extremity/should fractures
- 80% of delayed diagnoses required a change in therapy, most commonly a sling or cast. 15% required surgery.
- The long-term delayed diagnosis rate was 4%
Bottom line: Delayed diagnosis remains an issue in patient of all ages. The reported 4% rate subjectively seems about right to me. The most important lesson from this study is the extremely high percentage of delayed diagnoses that required further therapy. This is why it is so important to implement a specific system (the tertiary survey) to seek out these diagnoses.
A tertiary survey is a repeat head-to-toe physical exam and a review of all radiographic imaging performed to date. The trauma center should define the time interval from admission, and I recommend no more than 24-48 hours. We do not count any diagnoses found during this exam as being delayed. However, if a tertiary exam was not performed, or injuries are found after it was completed, we do consider it delayed an run it through our performance improvement process.
Related posts:
Reference: Ten-Year Retrospective Study of Delayed Diagnosis of Injury in Pediatric Trauma Patients at a Level II Trauma Center. Pediatric Emerg Care 25(8)-489-493, 2009.