For decades, plasma (with vitamin K) was the mainstay for reversing warfarin. Over the past several years, prothrombin complex concentrates (PCC) have made inroads in the management of this problem because of its sheer speed of action.
There are two problems with plasma. First, most hospitals still have only fresh frozen plasma (FFP), and it takes 20-30 minutes to thaw. This adds some up-front time to administration. Then, it takes time to infuse the 250cc or so of volume in each unit. This may be 1 or 2 hours, depending on policy and patient tolerance of a bolus of colloid.
If it always just took one unit of plasma to correct the INR to a desirable range (typically 1.5-1.6), then the whole PCC conversation might be moot. You could potentially have the INR corrected in 30-60 minutes depending on your patient’s cardiovascular system.
But how many does it really take? A group at Eastern Virginia Medical School in Norfolk, VA looked at this problem and tried to come up with a mathematical formula. They examined a year of warfarin reversal data at their hospital. Patients with severe clotting disturbances (advanced cirrhosis, DIC) and those who received additional products (PCC or activated Factor VII) were excluded.
Using data from nearly 1,000 patients, the following formula was derived and validated:
∆ INR = (0.57 ∙ preINR) – 0.72
So a patient with an INR of 3.0 would be expected to show a decrease of 0.99 to about 2.0 after one unit. This formula can be used iteratively to figure out how many units will drop the INR to the goal range.
I don’t know about you, but I hate doing math in the middle of a trauma resuscitation. I need something quick and dirty. A physician from NYU Langone in NYC commented on the article, and derived a nice little table to simplify the process. He calculated the number of plasma units based on some common INR ranges, assuming that the goal was to get it down under 1.5. Here is the table:
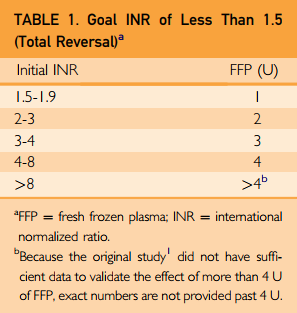
Bottom line: This is a nice little piece of information to tuck into your pocket or phone. For patients inside the usual therapeutic values, it will take 2-3 units of plasma to reverse. For your average older human with average comorbidities, expect this to take 4-6 hours, not counting ordering, thawing, and delivery. If my definitions of “life-threatening bleeding” are met (see below), your patient may have significant adverse events during this time frame. So think very seriously about using PCC instead.
Related posts:
Reference: Fresh Frozen Plasma Dosing for Warfarin Reversal: A Practical Formula. Mayo Clin Proc 88(3):244-250, 2013.