In my last two posts, I reviewed who is at risk for blunt carotid / vertebral injury (BCVI) and how to find it. But what does it actually look like, and how is it classified?
A seminal paper from Denver Health (aka Denver General Hospital) in 1999 proposed the most commonly used grading system for BCVI. This Denver scale should not be confused with the Denver criteria that predict risk for BCVI. Here’s a nice graphic that explains the classifications:
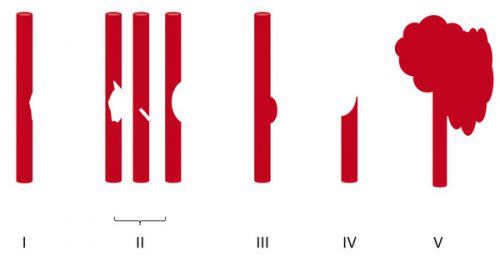
Grade I: A mild intimal irregularity is seen. Note the abnormal narrowed area, representing a small intimal injury, possibly with a small amount of clot.
Grade II: This grade has several presentations. There may be a intraluminal thrombosis/hematoma with (left) or without (right) an intimal flap, or a flap alone (center)
Grade III: There is a full-thickness injury to the vessel with a contained extraluminal extravasation (pseudoaneurysm)
Grade IV: The vessel is completely occluded by flap or thrombus
Grade V: The artery is transected and freely extravasating
In the next post, I’ll finish off with a summary of the treatments for these injuries.
Reference: Blunt carotid arterial injuries: implications of a new grading scale. J Trauma. 47(5): 845-53, 1999.
