Pediatric trauma centers have an excellent reputation when it comes to caring for children when compared to their adult counterparts. Overall mortality for major trauma is lower. Splenectomy rates and the use of angiography are less in children with solid organ injury. And because of this expertise, it is common for surrounding trauma centers of all levels transfer these patients to the nearest pediatric trauma center.
But is this always necessary? Many of these children have relatively minor injury, and the pediatric trauma centers can be few and far between unless you are on one of the coasts. Researchers at the University of Washington, Harborview, and Seattle Children’s looked at their experience with pediatric transfers (or lack thereof) with spleen injury.
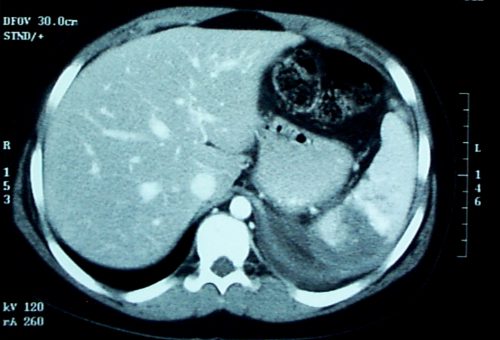
They retrospectively looked at 15 years of transfer data. The Seattle hospitals are the catchment area for a huge geographic area in the northwest, and the state trauma system maintains detailed records on all transfers to a higher level of care. Patients 16 years or younger with low grade (I-III) spleen injury were included. In an effort to narrow the focus to relatively isolated spleen injury, patients were excluded if they had moderate injuries in other AIS body regions.
Here are the factoids:
- During the study, over 54,000 patients were admitted to hospitals, but only 1,177 had isolated, low grade spleen injury
- About 20% presented directly to a Level I or II trauma center, 30% presented to a lower level center and were transferred, and 50% stayed put at the lower level center they to which they presented
- 40 patients (3%) underwent an abdominal operation presumably for their spleen, but there was no difference based on which hospital they presented to or whether they were transferred
- The incidence of total splenectomy was not different among the three groups
- Likewise, there was no difference in ICU admission or ICU length of stay
- The only significant difference was that patients who were not transferred to a pediatric center usually spent an extra day in the hospital
Bottom line: Injured children tend to do well, regardless of where they are treated. This study is huge and retrospective, which can cause analysis problems. And even given the size, the total number eligible for the study was relatively small. But it is the best study to date that shows that it is possible to treat select low grade injuries at non-pediatric, non-high level trauma centers. However, before going down this path, it is extremely important to define specific “safe” injuries to manage, and to have an escape valve available in case the patient takes an unexpected turn.