The Eastern Association for the Surgery of Trauma is in the process of updating their trauma practice guidelines for spleen injury. The first set of guidelines was introduced in 2003, and several advances in management have occurred since. here is a summary of the current status of the guidelines:
Level I recommendations (best quality data):
- none
Level II recommendations (good data):
- Initial management of hemodynamically stable patients should be nonoperative
- Unstable patients should undergo immediate operation or angiographic embolization (my interpretation: unstable patients belong in the OR, not the angio suite!)
- Patients with peritonitis should go to the operating room
- Age, grade of injury, amount of hemoperitoneum and age are not contraindications to nonoperative management. Only hemodynamic stability matters.
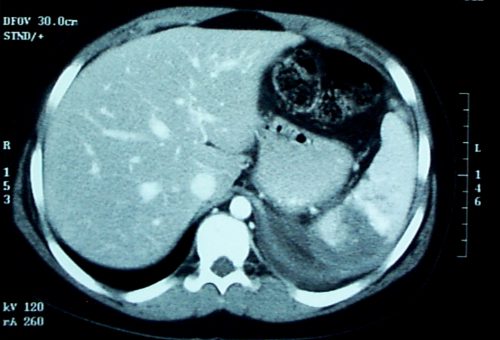
- CT of the abdomen with IV contrast is the most reliable method to assess severity of spleen injury (my interpretation: in the hemodynamically stable patient)
- Angiography with embolization should be considered if a contrast blush is seen on CT, AAST grade > 3, moderate hemoperitoneum is present, or there is evidence of ongoing bleeding
- Nonoperative management should only be considered if continuous monitoring and serial exams can be carried out at your hospital, and if an operating room is immediately available if needed
Level III recommendations (weak data):
- Clinical status should dictate need and frequency of followup imaging (my interpretation: only do it if the patient condition changes for the worse)
- Contrast blush is not an absolute indication for operation or angio-embolization. Age, grade of injury and presence of hypotension need to be considered. (My interpretation: don’t operate or do angio on kids without a really good reason)
- Angio is an adjunct to nonop management in patients who are at high risk for delayed bleeding or to look for vascular injuries (pseudoaneurysms) that may lead to rupture or delayed hemorrhage
Reference: Trauma Practice Guideline Update, 24th Annual Scientic Assembly, Eastern Association for the Surgery of Trauma, January 2011.