In my last post, I detailed the following case:
This male patient was brought to the trauma center after a high-speed car crash. He was unresponsive with GCS 3. A bleeding facial laceration was present, as was vomitus in the airway.
Prehospital providers rapidly intubated the patient and inserted an orogastric tube. They rapidly packaged and transported him to the nearest trauma center. The facial laceration was stapled for bleeding control. The airway was checked with a CO2 color change indicator and was positive. OG was hooked to suction with return of gastric contents.
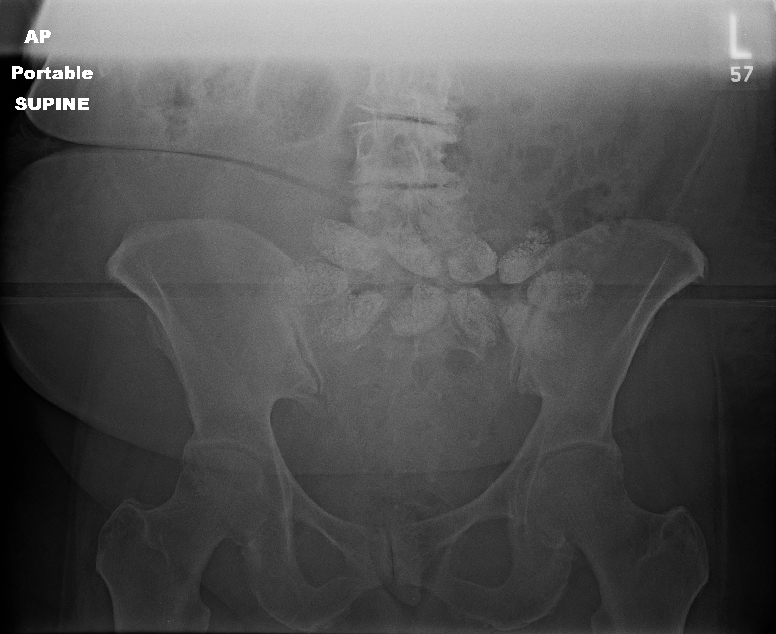
And here was a lateral cervical spine image:

The main problem is that, if you look closely there are three tubes on the image!
Look carefully at the anterior pharynx and trace the radiopaque markers back. There are two nearly overlapping lines. One extends posteriorly, down into the esophagus. This is the orogastric tube. The distal tip of the other (an endotracheal tube which is only inserted to 12 cm at the teeth) stops where it touches another tube. Another endotracheal tube, the proximal end of which is sitting at the epiglottis!
What the heck??! The medics were interviewed, and the patient was initially intubated successfully. The intubator turned his attention to finding a tube securing device, and when he turned back the tube was gone! So he intubated again but met some resistance. This explained the shallow position of the tube.
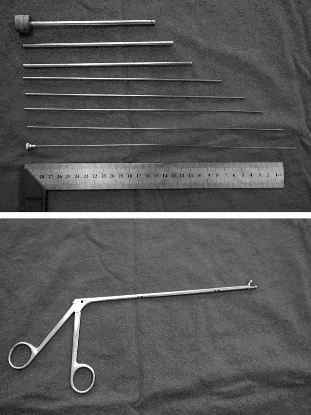
The patient was oxygenated well and the “outside” ET tube was removed. Then ring forceps were passed under direct vision and the “inside” tube was removed. A well-positioned ET tube was then reinserted. The patient did well afterwards.
Teaching point: When inserting anything that is partially in and partially out of the body (e.g. guidewires, and now ET tubes) always anchor them with your fingers so they don’t just “disappear.” And if you need more hands, ask for assistance!
Source: personal collection. Not treated at Regions Hospital or even in Minnesota.