Here is the fifth and final installment of my series summarizing the Austrian consensus paper on management of TBI patients with intracranial hemorrhage. The previous posts have run the gamut from diagnostic tests to detection of specific drugs to management. I’ve covered platelet inhibitors and Vitamin K antagonist reversal in previous posts, and today I’ll go over the panel’s reversal strategies for the direct oral anticoagulant drugs (DOACs).
Q1. Should idarucizumab (Praxbind) always be administered to patients with hemorrhagic TBI who are taking dabigatran (Pradaxa).
Answer: Only in cases where your laboratory is not capable of testing for thrombin time.
If thrombin time (TT) can be measured and is within the normal range, then the drug is not therapeutic and reversal should not be carried out. The consensus statement recommends giving this drug if the TT is prolonged or your lab cannot measure it. Keep in mind that there are very, very few papers on DOAC reversal in trauma patients. Most studies address the stroke population, and this may not translate well to trauma. And there are no studies yet that show that idarucizumab offers any survival benefit if given.
Q2. Should prothrombin complex concentrate (PCC) always be given to patients who are taking Factor Xa inhibitors?
Answer: Only in cases where your laboratory is not capable of testing for anti-Xa activity.
If anti-Xa activity can be measured (in a timely manner) and is low, then the drug is not therapeutic and PCC need not be given. If the level is high or your lab cannot test for it, then the group recommends administering PCC if the specific reversal agent (Andexxa) is not available.
As with dabigatran above, there is very little trauma literature to justify this recommendation. Furthermore, Andexxa is very expensive and, like idarucizumab, has not been shown to improve survival. Next week, I’ll write about why Andexxa is probably not worth the cost, in my opinion.
Q3. Should DOACs always be reversed in hemorrhagic TBI?
Answer: We don’t know.
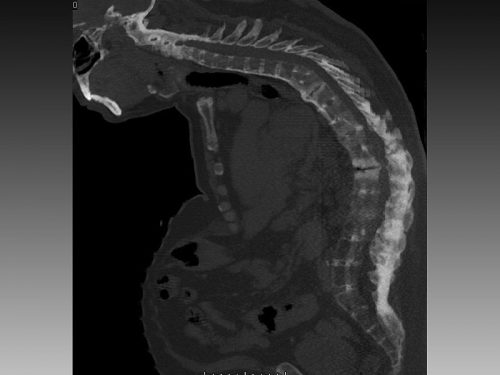
As I just mentioned, there is little if any data showing that administration of a reversal agent is beneficial. And the decision to give it must be balanced with patient risk for thrombosis and consideration of any other agents they may be taking. Expert opinion suggests that DOACs need not be reversed in TBI without blood on the CT scan, patients with unilateral, asymptomatic chronic subdural hematoma, and those with other wounds that do not appear to be bleeding excessively.
Hopefully, this series has helped shine some light on a confusing set of problems. Next week I’ll dig a bit deeper into the DOAC reversal agents Praxbind and Andexxa.
Reference: Diagnostic and therapeutic approach in adult patients with traumatic brain injury receiving oral anticoagulant therapy: an Austrian interdisciplinary consensus statement. Crit Care 23:62, 2019.