In my last post, I discussed a little-reviewed topic, that of strangulation. I recommended activating your trauma team only for patients who met the physiologic criteria for it.
But now, what about hangings? There are basically two types. The judicial hanging is something most of you will never see. This is a precisely carried out technique for execution and involves falling a certain height while a professionally fashioned noose arrests the fall. This results in a fairly predictable set of cervical spine/cord, airway, and vascular injuries. Death is rapid.
Suicidal hangings are far different. They involve some type of ligature around the neck, but rarely and fall. This causes slow asphyxiation and death, sometimes. The literature dealing with near hangings is a potpourri of case reports, speculation, and very few actual studies. So once again, we are left with little guidance.
What type of workup should occur? Does the trauma team need to be called? A very busy Level I trauma center reviewed their registry for adult near-hangings over a 19 year period. Hanging was strictly defined as a ligature around the neck with only the body weight for suspension. A total of 125 patients were analyzed, and were grouped into patients presenting with a normal GCS (15), and those who were abnormal (<15).
Here are the factoids:
- Two thirds of patients presented with normal GCS, and one third were impaired
- Most occurred at home (64%), and jail hangings occurred in 6%
- Only 13% actually fell some distance before the ligature tightened
- If there was no fall, 32% had full weight on the ligature, 28% had no weight on it, and 40% had partial weight
- Patients with decreased GCS tended to have full weight on suspension (76%), were much more likely to be intubated prior to arrival (83% vs 0% for GCS 15), had loss of consciousness (77% vs 35%) and had dysphonia and/or dysphagia (30% vs 8%)
- Other than a ligature mark, physical findings were rare, especially in the normal GCS group. Subq air was found in only 12% and stridor in 18%.
- No patients had physical findings associated with vascular injury (thrill, bruit)
- Injuries were only found in 4 patients: 1 cervical spine fracture, 2 vascular injuries, and 1 pneumothorax
- 10 patients died and 8 suffered permanent disability, all in the low GCS group
Bottom line: It is obvious that patients with normal GCS after attempted hanging are very different from those who are impaired. The authors developed an algorithm based on the initial GCS, which I agree with. Here is what I recommend:
- Do not activate the trauma team, even for low GCS. This mechanism seldom produces injuries that require any surgical specialist. This is an exception to the usual GCS criterion.
- The emergency physician should direct the initial diagnosis and management. This includes airway, selection of imaging, and directing disposition. A good physical exam, including auscultation (remember that?) is essential.
- Patients with normal GCS and minimal neck tenderness or other symptoms do not need imaging of any kind.
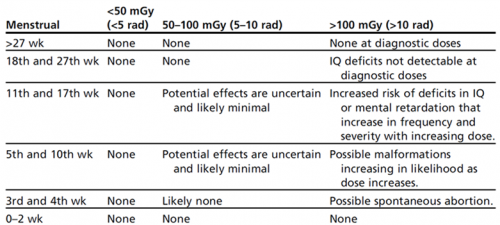
- Patients with abnormal GCS should undergo CT scanning, consisting of a CT angiogram of the neck and brain with soft tissue images of the neck and cervical spine recons.
- Based on final diagnoses, the patient can be admitted to an appropriate medical service or mental health. In the very rare case of a spine, airway, or vascular injury, the appropriate service can be consulted.
Reference: A case for less workup in near hanging. J Trauma 81(5):925-930, 2016.