Most emergency departments do not see much penetrating trauma. But it is helpful to be able to learn as much as possible from the appearance of these piercing injuries when you do see them. This post will describe the basics of reading stab wounds.
Important: This information will allow some basic interpretation of wounds. It will not qualify you as a forensics expert by any means. I do not recommend that you document any of this information in the medical record unless you have specific forensic training. You should only write things like “a wound was noted in the midepigastrium that is 2 cm in length.” Your note can and will be used in a court of law, and if you are wrong there can be significant consequences for the plaintiff or the defendant. This information is for your edification only.
1. What is the length of the wound? This does not necessarily correspond to the width of the blade. Skin stretches as it is cut, so the wound will usually retract to a length that is shorter than the full width of the blade.
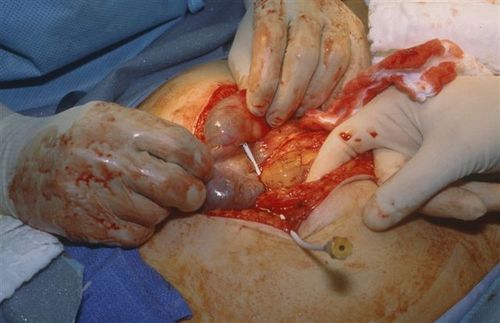
2. Is the item sharp on one side or both? This can usually be determined by the appearance of the wound. A linear wound with two sharp ends is generally a two sided knife. A wound with one flat end and one sharp end is usually from a one-sided weapon. The picture below shows a knife wound with one sharp side.

3. Is there a hilt mark? This can usually be detected by looking for bruising around the wound. The picture below shows a knife wound with a hilt mark.

4. What is the angle? If both edges are symmetric, the knife went straight in. If one surface has a tangential appearance, then the knife was angled toward that side. You can approximate the direction of entry by looking at the tangential surface of the wound edge. In this example, the blade is angling upward toward the right.

5. How deep did it go? You have no way of knowing unless you have the blood stained blade in your possession. And yes, it is possible for the wound to go deeper than the length of the knife, since the abdominal wall or other soft tissues can be pushed inwards during the stab.