Blunt cardiac injury (BCI), better known as cardiac contusion, has been poorly understood for decades. There has always been confusion about the best way to detect, monitor, and treat this condition. The Eastern Association for the Surgery of Trauma developed a set of practice guidelines in 1998 that provided solid, evidence-based principles to act upon. At that time, CPK was the only cardiac enzyme available. It was useless because it had no correlation with presence or absence of contusion, or even severity of injury.
With the arrival of troponin assays, a new tool for looking at cardiac injury became available. However, initial evaluations indicated that it was also not very reliable when used in the diagnosis of cardiac contusion. For years, I’ve been teaching that these enzymes are useless. However, additional work has been done that does show some limited usefulness.
A prospective study by Collins looked at the usefulness of troponin I (TnI) in patients with cardiac injury. As in previous retrospective studies, this test had a very low positive predictive value. In addition, they determined that a negative EKG alone ruled out blunt cardiac injury. So what good is it?
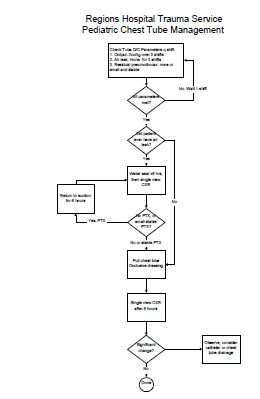
The new piece of information here is that if the EKG is abnormal and the troponin I is normal, then a cardiac contusion can be ruled out. This changes the overall algorithm by allowing us to eliminate some patients who have abnormal EKGs.
On Monday, I’ll provide my take on a comprehensive algorithm for evaluating and managing cardiac injury. Stay tuned.
Related posts:
Reference: The usefulness of serum troponin levels in evaluating cardiac injury. Am Surg 67:821-826, 2001.