Yesterday I gave a little perspective on the use of CT in assessing the diaphragm after penetrating injury. Today, I’ll break it down into some practical steps you can follow the next time you see one.
Step 1. Stable or unstable? If your patient arrives with unstable vital signs, and there is no other source but the abdomen, the answer is simple. Go to the OR for a laparotomy. Period. They are exsanguinating and the hemorrhage needs to be stopped.
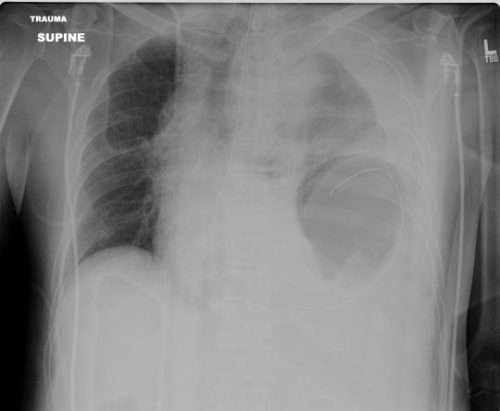
Step 2. Mark the sites of penetration and take a chest x-ray. This will let you evaluate the potential trajectory of the object, and will give you your first glimpse of the diaphragm.
Step 3. Examine the abdomen. Actually, you should be doing this at the same time you are setting up for Step 2. If your patient has peritoneal signs, no further evaluation is needed. Just go to the OR for laparotomy. Look at the chest x-ray once you get there.
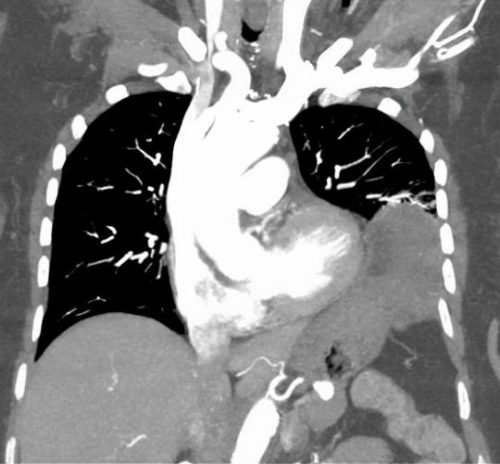
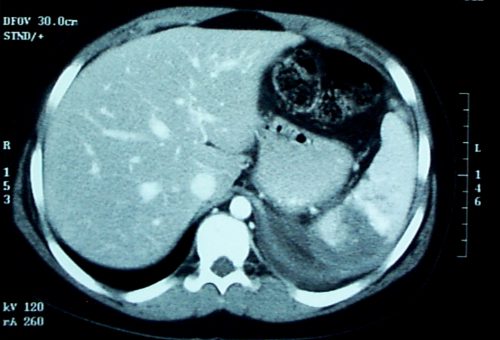
Step 4. Right side? If your appreciation of the path of penetration involves just the liver, take the patient to CT for evaluation of chest, abdomen, and pelvis. You need to see all three of these areas to assess for blood and fluid in both body cavities. After the study, if you still think the injury is limited to the liver, admit the patient for observation.
Step 5. Left side? Look at that chest x-ray again. If there are any irregularities at all, strongly consider going to the OR and starting with diagnostic laparoscopy. These irregularities can be glaring, like in the x-ray above. But they can be subtle, like some haziness above the diaphragm or small hemothorax. Obviously, if the injury is as clear as on the x-ray above, just open the abdomen. But if in doubt, start small. And remember my advice on “lunchothorax.”
Step 6. Admit and observe. Check the abdomen periodically, and repeat the chest x-ray daily. If anything changes, consider diagnostic laparoscopy. As a general rule, I don’t keep patients NPO “just in case.” Most will pass this test, and I don’t see a reason to starve my patients for the low likelihood they need to go to the OR.
Step 7. Make sure your patient gets a follow up evaluation. See them in your outpatient clinic, get a final chest x-ray and abdominal exam before you completely clear them.