Inserting an NG Tube (Not an NC Tube)!
On occasion (but not routinely) trauma patients need to have their stomach decompressed. The reflex maneuver is to insert a nasogastric (NG) tube. However, this may be a dangerous procedure in some patients.
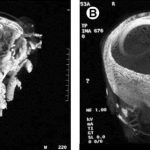
Some patients may be at risk for a cribriform plate fracture, and blindly passing a tube into their nose may result in a nasocerebral (NC) tube (see picture). This is a neurosurgical catastrophe, and the outcome is uniformly dismal. It generally requires craniectomy to remove the tube.
The following patients are at risk:
- Evidence of midface trauma (eyebrows to zygoma)
- Evidence of basilar skull fracture (raccoon eyes, Battle’s sign, fluids leaking from ears or nose)
- Coma (GCS<8)
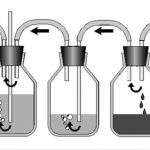
If you really need the tube, what can you do? If the patient is comatose, it’s easy: just insert an orogastric (OG) tube. However, that is not an option in awake patients; they will continuously gag on the tube. In that case, lubricate a curved nasal trumpet and gently insert it into the nose. The curve will safely move it past the cribriform plate area. Then lubricate a smaller gastric tube and pass it through the trumpet.