Two years ago, an abstract was presented at this meeting describing the concept of the “hybrid ER.” Check it out using this link. This concept was pioneered in Japan, and consists of a special trauma resuscitation room in the ED with everything but an operating room built into it. It’s possible to perform whole-body CT scan, interventional procedures, and REBOA without moving the patient. Here’s a picture from that abstract:
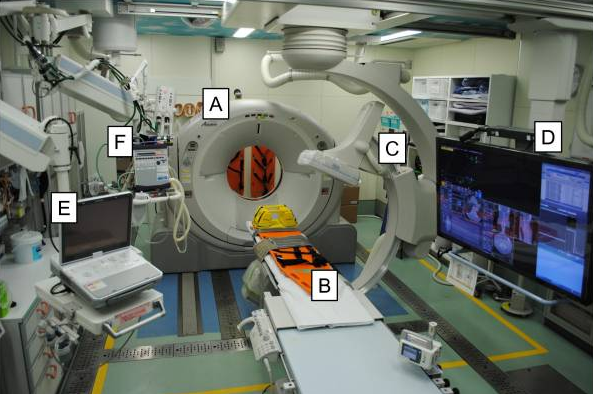
A = CT scanner B = CT exam table C = movable C-arm D = monitor screen E = ultrasound F = ventilator
In that abstract, about a thousand patients were compared with two thirds in the hybrid ER group and one third undergoing conventional evaluation. The authors concluded that mortality was significantly improved in the hybrid ER group, and even more so in high ISS patients.
I had a lot of questions for that abstract that were answered in the subsequently published manuscript (reference 2). The authors have updated their experience using new data from the last five years. They created a new approach to resuscitation that is different than the usual ATLS sequence for select patients. Here’s the algorithm they used:
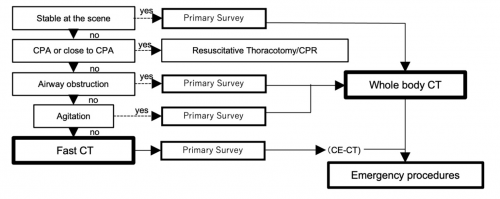
The primary survey is completed, then the patient undergoes a quick whole body CT scan. After that, the secondary survey progresses and any necessary emergency procedures are performed.
In this abstract, the authors compared a group of 46 patients who underwent standard ATLS evaluation with 49 who received the expedited process, which they termed CT First Resuscitation (CTFR). All patients had presumptive hemorrhagic shock based on prehospital vital signs. The authors analyzed injury patterns, interventions performed, timing, adverse events, and outcome. Demographics and injury severity were similar in the two groups.
Here are the factoids:
- Time to CT in the CTFR group was significantly shorter (1.5 min vs 15 min)
- The expedited scan settings for CTFR resulted in blindingly fast scan times (median 56 seconds)
- None of the CTFR patients decompensated during the scan process
- There was no difference in mortality between CTFR and standard evaluation (14% vs 4%, p=.1)
- There was no difference in time to hemostatic intervention (56 vs 59 minutes)
- There was no difference in red cell transfusions (no units in either group)
The authors concluded that CTFR expedited trauma management without adverse effects, and there was no increase in mortality. They, or course, recommended further study.
Bottom line: Several trauma surgeons from a variety of centers wrote an invited commentary last year (reference 3) expressing their excitement about this concept. Reducing time to definitive control of hemorrhage has been repeatedly shown to improve survival. The hybrid ER is one way of reducing those times by eliminating most of the time needed to move the patient about and providing everything but an operating room in the emergency department.
But they also recognized the limitations of this concept. The changes to the ED physical plant are extreme and involve the installation of very expensive equipment that must be heavily shielded from the rest of the emergency department. There are also significant differences in physician training and hospital reimbursement between Japan and the US. This will probably severely limit the adoption of this technology in the States.
I believe that this is an important study showing the feasibility of this method of evaluation. Unfortunately, it does not allow us to draw any real conclusions about safety and efficacy due to the low numbers of patients enrolled. I agree with the authors that a larger study should be performed so we can truly determine whether this concept can possibly be applied outside of Japan.
Here are my questions for the authors / presenter:
- Did you perform a power analysis? I doubt that the sample size reported would allow for any findings of statistical significance with the exception of huge differences like time to CT.
- How do you protect the trauma team from radiation exposure? Since these patients are in shock when they arrive, I assume that the team cannot leave the room. CT scan radiation exposure of the team is significantly higher than a chest and pelvis x-ray. Repeated team exposure may pose risks.
- Does the trend toward higher mortality in the CTFR group trouble you? Sure, it is not statistically significant. But it is approaching significance with a small sample group.
- Why didn’t the CTFR group have more rapid hemostatic intervention? One would think these early results could help move the patient to an OR more quickly. And why did it take an hour? Isn’t that a long time?
- Why didn’t your patients receive any blood? Weren’t they supposed to be at risk for hemorrhagic shock? How did you treat it without blood? Perhaps your selection criteria need to be tweaked.
This is a nice follow on study from the previous presentation two years ago. It could be an exciting advance in resuscitation, but we need much more info to pass judgement. I’m looking forward to the presentation.
References:
- COMPUTED TOMOGRAPHY FIRST RESUSCITATION WITH HYBRID EMERGENCY ROOM FOR SEVERELY INJURED PATIENTS. Plenary paper #25, AAST 2022.
- Hybrid emergency room shows maximum effect on trauma resuscitation when used in patients with higher severity. J Trauma Acute Care Surg. 2021 Feb 1;90(2):232-239.
- Time to Hemorrhage Control in a Hybrid ER System: Is It Time to Change? Shock. 2021 Dec 1;56(1S):16-21.

