In my last post, I reviewed a simple technique utilizing a reminder card and provider feedback loops to reduce deep intubations in pediatric patients. Today, I’ll review three other techniques and discuss a paper that compared their efficacy.
A variety of techniques for determining and/or confirming endotracheal tube position exist. Use of one or more of them is important in children due to their short trachea and increased likelihood of deep intubation. Some, like the confirmatory chest x-ray, are obvious. However, it’s more desirable to apply techniques during the intubation in order to avoid deep intubation in the first place. Hyperinflation of one lung, especially in very small children, can cause a host of impairments and complications that may compound their other injuries.
A paper from the University Hospital Basel in Switzerland evaluated three techniques: bronchoscopic insertion to a specific depth, cuff palpation in the sternal notch, and intentional right mainstem intubation followed by slow withdrawal during auscultation. Each of 68 children ranging in age from 0 to 4 years were studied using all three techniques.
Each endotracheal tube was marked at the ideal insertion point that would ideally be placed just beyond the vocal cords. The distance from this mark to the mouth end of the tube was measured so actual intubation depths could be compared.
Bronchoscopic insertion was always performed first to obtain a baseline depth measurement, essentially the gold standard. The other two techniques were performed in random order. For the cuff palpation technique, the trachea was palpated while the balloon was intermittently partially inflated until it could be felt at the suprasternal notch. For the mainstem intubation technique, the uninflated tube was advanced until breath sounds in the left axilla disappeared. It was then slowly withdrawn until sounds reappeared.
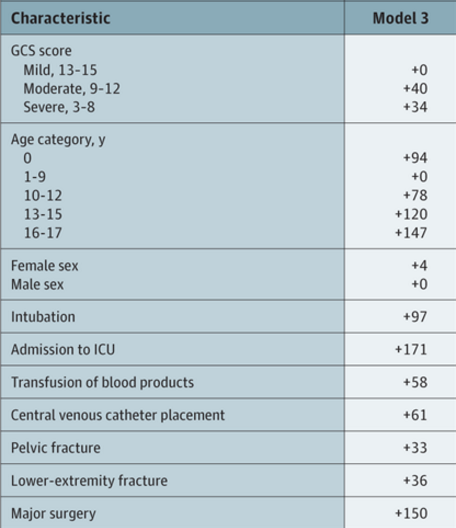
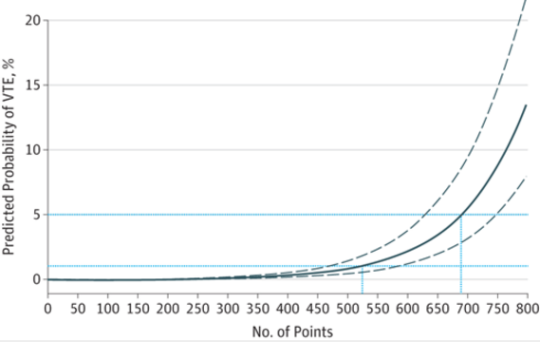
Distances from the tip of the tube to the carina was calculated using the insertion depth at the incisors and the initial ideal intubation depth mark. Here are the factoids:
- Insertion to a depth mark on the tube via bronchoscope technique resulted in the highest tube tip with respect to the carina, and also with the greatest depth variability
- The cuff palpation technique resulted in less distance to the carina (about 19mm vs 36 for the mark technique) and less variability
- Use of the mainstem intubation with pullback technique resulted in the tube tip resting within just a few mm of the carina, but tube depth was very consistent
Bottom line: What to make of all this? Which technique is “best?” First, it’s not practical or advisable to use a bronchoscope for every pediatric intubation. It’s invasive and adds complexity and time to a critical procedure. The cuff palpation technique also takes additional time due to the repeated cuff inflation/deflation that is required. However, the tube position is fairly accurate and safe.
The intentional right mainstem intubation with pull-back seems a bit sketchy. It requires some type of ongoing ventilation while the tube is being inserted, as well as someone who can listen to the left chest. Additionally, it results in a tube position that is so low that neck positioning may move it into the mainstem bronchus again.
In my mind, estimation of the proper depth pre-intubation is probably the best. Strict attention must be paid to the final depth of the tube once it is inserted, as measured by the distance marker at the incisors. This number must match the one decided upon at the start of the procedure. A good exam of the chest should be carried out to quickly identify an inadvertent mainstem intubation. And finally, a quick confirmatory chest x-ray should always be obtained for objective information on tube position.
The fancy techniques described in this paper add too much time and complexity for intubation in a trauma situation. They may very well have a place in the OR where the situation is more controlled and there is more advanced equipment and support. But stick to the basics when intubating children in your trauma bay!
Reference: Assessment of three placement techniques for individualized positioning of the tip of the tracheal tube in children under the age of 4 years. Ped Anesthesia 25:379-285, 2014.