Here’s a brief video from one of the device manufacturers that illustrates the technique of duplex ultrasound in the lower extremity.
Monthly Archives: May 2017
Duplex Ultrasound For DVT: How Does It Work?
Admit it. You’re curious. You order this test for your trauma patients all the time but you’ve never seen it done. It’s simple and noninvasive, but it does require access to all areas to be evaluated. This means that extremities that are casted or splinted, or that have extensive dressings in place may be incompletely evaluated.
The study is called “duplex” because it makes use of two modalities: traditional ultrasound and Doppler ultrasound. Traditional ultrasound is used to view the compressibility of the veins of interest at a number of locations. Doppler measures the speed of blood flow under the probe, and can show areas of sluggish flow.
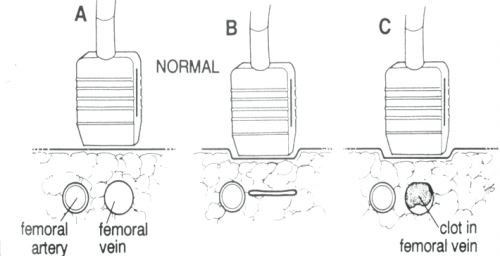
The following diagram shows the traditional ultrasound technique being used to compress the vein of interest (femoral, popliteal, etc.). Part A shows the probe gently resting over the vessels. Part B shows a fully compressible vein (normal), and Part C shoes partial compression due to the presence of thrombus.
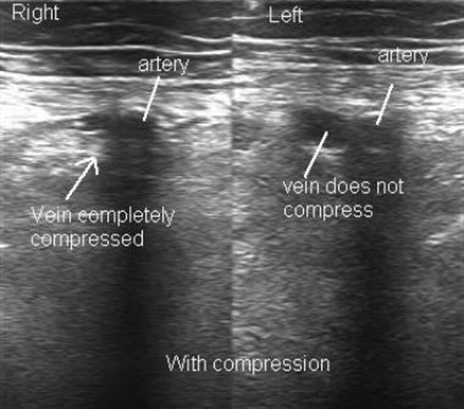
The following diagram shows what the actual ultrasound study looks like. The right side is normal, but the left side shows a venous thrombosis.
Aspirin For DVT Prophylaxis In Trauma
The use of mechanical and pharmacologic prophylaxis for prevention of deep venous thrombosis (DVT) and venous thromboembolism (VTE) in trauma patients is nearly universal. However, no matter how closely we adhere to existing guidelines, some patients will develop these conditions. Indeed, about 80% of patient who suffer some type of VTE event were receiving prophylaxis at the time.
Trauma is a major factor in causing hypercoagulability. Although current chemoprophylaxis focuses on clotting factors, platelets play a big part in the clot formation process. Our usual drugs, though (various flavors of heparin), have no effect on them.
What about adding aspirin to the regimen? My orthopedic colleagues have been requesting this for years. There is a reasonable amount of data in their literature that it is effect in patients with knee arthroplasty only. As usual, it is misguided to try to generalize management based on experience from one specific body region or operation.
A single Level I trauma center reviewed its data on aspirin prophylaxis for trauma patients. They reviewed their registry data from 2006 to 2011. They identified 172 trauma patients with duplex ultrasound proven DVT. These patients were matched with 1,901 control patients who underwent at least one duplex and never developed DVT. Matching was performed carefully to ensure that age, probability of death, number of DVT risk factors, and presence of TBI were similar. The total number of matched patients studied was 110.
And here are the factoids:
- About 7% of patients with DVT were on aspirin at the time of their injury, vs 14% of the matched controls
- 7% were taking warfarin, and 4% were taking clopidogrel
- Analysis showed that patients taking aspirin had a significantly decreased chance of DVT after injury
- On further analysis, it was found that this effect was only significant if some form of heparin was given for prophylaxis as well.
Bottom line: So before you run off and start giving your patients aspirin, think about what this study really said. Patients taking aspirin before their injury and coupled with heparin after their injury have a lower rate of DVT. It gives us no guidance as to whether adding aspirin after the fact, or using aspirin alone, are useful. And we still don’t know if any of this decreases pulmonary embolism or mortality rates.
Related posts:
- Below knee DVT: worse than we thought
- DVT prophylaxis interruptus
- DVT prophylaxis after solid organ injury
Reference: Aspirin as added prophylaxis for deep vein thrombosis in trauma: a retrospective case-control study. J Trauma 80(4):625-30, 2016.
What’s Wrong With My Patient? Final Answer!
I previously described a young man who was recovering from surgery for repair of a stab to the heart. He presented shortly after discharge with fever, a slightly elevated WBC, some EKG changes, and a small pericardial effusion.
Several people tweeted out the answer, which is post-pericardiotomy syndrome (PPS).
PPS is an inflammatory reaction to traumatic and then surgical injury to the pericardium. It is seen in a relatively small percentage of patients who undergo pericardiotomy for trauma, which is why patients who develop it are such a surprise to trauma professionals. A similar condition can develop after myocardial infarction (Dressler syndrome) and was first described in 1956. The classic paper describing PPS after trauma was published five years later (cited below).
Symptoms typically develop 1-6 weeks after surgery, and usually consist of low grade fevers, malaise, chest pain, and occasionally arthralgia. A pericardial friction rub may be present (and where is that stethoscope, BTW?). The WBC is usually elevated, with some degree of left shift. EKG may show some degree of pericarditis, including global ST elevation and T wave inversion.
Chest x-ray is usually nonspecific, but may show pleural effusion or an enlarged heart due to the presence of some pericardial fluid. Ultrasound may confirm a pericardial effusion, but this is not a reliable finding since the pericardium is typically left open at the end of the operation.
Treatment is symptomatic, usually consisting of NSAIDS or aspirin to tone down the inflammatory response. These drugs are usually given for 4-6 weeks, then tapered. If the effusion is large, pericardiocentesis may be needed.
Bottom line: If your postop heart injury patient presents with these symptoms, consider infectious etiologies first, but remember that they are typically even less common than post-pericardiotomy syndrome. Reassure your patient, then reach for the ibuprofen to get them through it.
Reference: Postpericardiotomy syndrome following traumatic hemopericardium. Am J Cardiology 7(1):83-96, 1961.

