I’ve watched it happen for years. A trauma patient is admitted with a small subarachnoid hemorrhage in the evening. The residents put in all the “usual” orders and tuck them away for the night. I am the rounder the next day, and when I saunter into the patient’s room, this is what I find:

They were made NPO. And this isn’t just an issue for patients with a small head bleed. A grade II spleen. An orbital fracture. Cervical spine injury. The list goes on.
What do these injuries have to do with your GI tract?
Here are some pointers on writing the correct diet orders on your trauma patients:
- Is there a plan to take them to the operating room within the next 8 hours or so? If not, let them eat. If you are not sure, contact the responsible service and ask. Once you have confirmed their OR status, write the appropriate order.
- Have they just come out of the operating room from a laparotomy? Then yes, they will have an ileus and should be NPO.
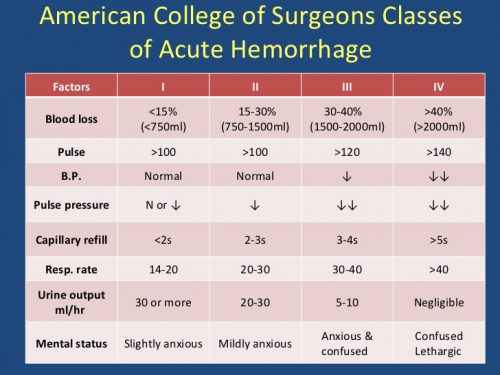
- Are they being admitted to the ICU? If their condition is tenuous enough that they need ICU level monitoring, then they actually do belong to that small group of patients that should be kept NPO.
But here’s the biggest offender. Most trauma professionals don’t think this one through, and reflexively write for the starvation diet.
- Do they have a condition that will likely require an emergent operation in the very near future? This one is a judgment call. But how often have you seen a patient with subarachnoid hemorrhage have an emergent craniotomy? How often do low grade solid organ injuries fail if they’ve always had stable vital signs? Or even high grade injuries? The answer is, not often at all! So let them eat!
Bottom line: Unless your patient is known to be heading to the OR soon, or just had a laparotomy, the default trauma diet should be a regular diet!