A few papers have been published in the nursing
literature about the detrimental effects of interruptions experienced during
patient care. Unfortunately, these papers have never taken the next step to
determine why they occur, and what steps can be taken to decrease the frequency
of this problem.
A group at Wright State in Dayton OH tried to
tease apart the various aspects of this issue. They observed registered nurses
in a 23 bed SICU at a Level I trauma center. A total of 25 sessions covering 75
hours and multiple nurses were analyzed for the cause and duration of any interruption,
and whether it caused a switch from their primary task.
Here are the factoids:
- Nurses were interrupted every 18
minutes on average - The dominant location was in the patient room (58%), and the most
common activity interrupted was documentation - Interruption by an attending or resident was less frequent (10%), but
ended up being longer than interruptions by other nurses (3 mins vs 1 min) - Interruptions of longer duration more commonly
caused the nurse to switch tasks
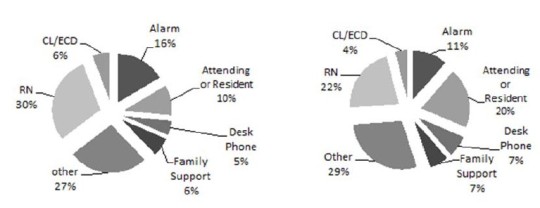
Frequency (left) and duration
(right) of interruptions from each source. CL = call light, ECD = electronic
communication device
Bottom
line: This is a first look at the anatomy of nursing interruptions in the SICU.
They are much more common than you think. Task switching (either mentally or
physically) is something that humans do poorly. It always degrades performance,
and can ultimately lead to patient harm. Hopefully, operational protocols can
be developed to protect nurses from unnecessary or non-urgent interruptions to
improve quality of care.
Reference:
The anatomy of nursing interruptions in a surgical intensive care unit at a
trauma center. EAST 2016 Poster abstract #18.