Admit it. It’s happened to you. You get paged to a trauma activation, hustle on down to the ED, and get dressed. The patient is calmly and comfortably lying on a cart, staring at you like you’re from Mars. Then you hear the story. He has a grade V spleen injury. But he just got back from CT scan. And his car crash was yesterday!
Is this appropriate? The answer is no! But, as you will see, the answer is not always as obvious as this example. The top thing to keep in mind in triggering a trauma activation appropriately is the reason behind having them in the first place.
The entire purpose of a trauma activation is speed. The assumption must be that your patient is dying and you have to (quickly) prove that they are not. It’s the null hypothesis of trauma.
Trauma teams are designed with certain common features:
- A group of people with a common purpose
- The ability to speed through the exam and bedside procedures via division of labor
- Rapid access to diagnostic studies, like CT scan
- Availability of blood products, if needed
- Immediate access to an OR, if needed
- Recognition in key departments throughout the hospital that a patient may need resources quickly
Every trauma center has trauma activation triage criteria that try to predict which patients will need this kind of speed. Does the patient in the example above need this? NO! He’s already been selected out to do well. Why, he’s practically finished the nonoperative solid organ management protocol on his own at home.
Here are some general rules:
- If the patient meets any of your physiologic and/or anatomic criteria, they are or can be sick. Trigger immediately, regardless of how much time has passed.
- If they meet only mechanism criteria and it’s been more than 6 hours since the event, they probably do not need the fast track.
- If they only meet the “clinician / EMS judgment” criteria, think about what the suspected injuries are based on a quick history and brief exam. Once again, if more than 6 hours have passed and there are no physiologic disturbances, the time for needing a trauma activation is probably past.
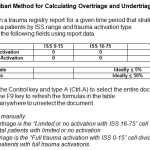
If you do decide not to trigger an activation in one of these cases, please let your trauma administrative team (trauma medical director, trauma program manager) know as soon as possible. This may appear to be undertriage as they analyze the admission, and it’s important for them to know the reasoning behind your choice so they can accurately document under- and over-triage.
Related posts: