It’s Also A Game!
There are not one, not two, but three Trauma Center games out for the Wii! Anyone try one of these out? If so, let’s hear some feedback!
It’s Also A Game!
There are not one, not two, but three Trauma Center games out for the Wii! Anyone try one of these out? If so, let’s hear some feedback!
Okay, so you’ve seen “other people” wearing perfectly good lead aprons lifting them up to their chin during portable xrays in the trauma bay. Is that really necessary, or is it just an urban legend?
After hitting the medical radiation physics books (really light reading, I must say), I’ve finally got an answer. Let’s say that the xray is taken in the “usual fashion”:
The calculated exposure to the patient is 52 microGrays. Most of the radiation goes through the patient onto the plate. A very small amount reflects off their bones and the table itself. This is the scatter we worry about.
So let’s assume that the closest person to the patient is 3 feet away. Remember that radiation intensity diminishes as the square of the distance. So if the distance doubles, the intensity decreases to one fourth. By calculating the intensity of the small amount of scatter at 3 feet from the patient, we come up with a whopping 0.2 microGrays. Since most people are even further away, the dose is much, much less for them.
Let’s put it perspective now. The background radiation we are exposed to every day (from cosmic rays, brick buildings, etc) amounts to about 2400 microGrays per year. So 0.2 microGrays from chest xray scatter is less than the radiation we are exposed to naturally every hour!
The bottom line: unless you need to work out you shoulders and pecs, don’t bother to lift your lead apron every time the portable xray unit beeps. It’s a waste of time and effort!
What kind of credentialing should the members of your trauma team have?
The most important concept in answering this question is based purely on patient care. What shows that your personnel can provide the type of care that their position on the team warrants?
For all physicians, ATLS is a must. Verification agencies, including the American College of Surgeons, require that most providers to have passed the course once. I recommend a current ATLS provider certificate for all physicians, including residents. The course is updated every four years, which means that every time a provider certificate expires, new course content has been added. A current certificate keeps their knowledge up to date.
The airway physician should be either credentialed or have generous experience in managing the airway. This ensures that the intubation process is routine and safe when necessary.
Most, if not all physicians should be also current in ACLS, since major trauma patients may arrest prior to or after arrival at the hospital.
Nurses involved in trauma resuscitations should have additional credentialing such as TNCC. They should also be current in ACLS, and many hospital have added critical care experience and ongoing training requirements related to trauma.
For pediatric trauma programs, a basic pediatric resuscitation course such as PALS or APLS is mandatory. All physicians and nurses taking care of critically injured children should be current so they can provide the best care possible to them.
A piece of paper does not necessarily prove competence. The final part of the qualification process involves your trauma Performance Improvement program. All providers are scrutinized by the PI process, and if any stand out as having too many adverse events to their name, they should not be allowed to participate on the team.
The bottom line: Your trauma team members need to be great at what they do, with appropriate paperwork to prove it and PI monitoring to back it up. They need to be able to easily pass the “family member” test: would I want this person to take care of my (daughter) (husband) (grandmother) etc!
Teaching hospitals have extra responsibilities when constructing their trauma activation team. They are typically charged with educating trainees from a variety of disciplines, including residents, medical students, and students from other disciplines (EMT, PA, NP). The activation process must not only provide rapid and high quality trauma care, it must also teach these students how to provide that care.
Residents can be integrated into the typical physician roles on the team: airway and primary examiner. To integrate more trainees, these roles can be split further. For example, the examiner’s role can be split into a primary examiner and a secondary examiner with separate, lesser responsibilities. PAs and NPs can be integrated into these roles as well.
One of the most important “additions” to the team that allows education of senior level residents is the Team Leader. This role allows the trainee to learn how to direct the overall resuscitation and allows them to practice making management decisions on the fly. Typically, the Team Leader does not actually touch the patient, allowing the other examining physicians to do this and learn their specific roles. Each role can be assigned to an appropriate level resident, so that they move to higher levels as they progress through their training program.
Here is a template for a trauma team that allows four trainees (yellow balloons) to participate. One faculty members supervises all of them.
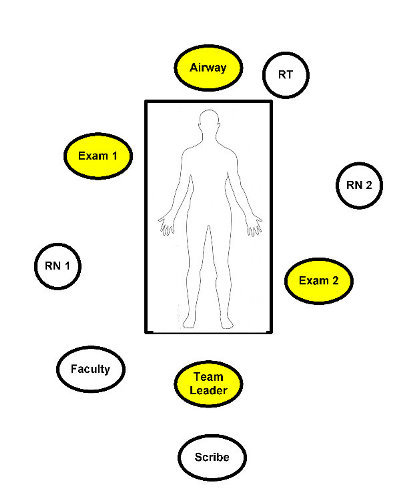
At our Trauma Center, we have these four trainees plus another Emergency Medicine resident who performs the FAST exam, if indicated. Two faculty members participate, one trauma surgeon and one Emergency Medicine faculty. Our total team size is 12, so it must be well-coordinated in order to avoid chaos.
Medical and paramedic students are usually confined to the periphery to take notes (H&P) or just observe.
Please leave your comments describing the composition of your team and what makes it run well.
Tomorrow: qualifications of your trauma team personnel
Yesterday’s video highlighted members of the trauma team at a medium size teaching hospital. Today, I will discuss who actually needs to be on the team.
The decisions leading to the composition of your trauma activation team are complex ones. The key is to look at your needs during a typical trauma resuscitation, and look at the resources available within the ED and the hospital as a whole.
The trauma resuscitation team can consist of as few as 4 to as many as 15 or more people! The first item to consider is who is available to go to a trauma activation? If your ED staff is small, the team will be small, or you will have to draw personnel from other areas of the hospital.
The absolute minimum personnel are:
Using the minimum contingent will force the use of ATLS the way it is classically taught, with the physician sequentially going through the entire process. Additional physicians and nurses allow overlapping portions of the evaluation and treatment and will also speed up the resuscitation process.
An ideal team for a non-teaching hospital is:
This allows for the physicians and nurses to split their responsibilities (airway, exam, IV access, monitoring) and assures adequate help with patient safety, evaluation and restraint.
Additional personnel can be added from outside the ED to provide a better interface with other hospital services. Examples include:
Tomorrow: trauma teams in the teaching hospital