Injury can be a bloody business, and trauma professionals take replacement of blood products for granted. Some patients object to this practice on religious grounds, and their health care providers often have a hard time understanding this. So why would someone refuse blood when the trauma team is convinced that it is the only thing that may save their life?
Jehovah’s Witnesses are the most common group encountered in the US that refuse transfusion. There are more than 20 million Witnesses worldwide, with over 7 million actively preaching. It is a Christian denomination that originated in Pennsylvania during the 1870s.
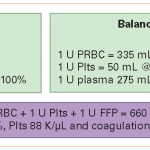
Witnesses believe that the bible prohibits taking any blood products, including red cells, white cells, platelets or plasma. It also includes the use of any dialysis or pump equipment that must be primed with blood. This is based on the belief that life is a gift from God and that it should not be sustained by receiving blood products. The status of certain prepared fractions such as albumin, factor concentrates, blood substitutes derived from hemoglobin, and albumin is not clear, and the majority of Witnesses will accept these products. Cell saver techniques may be acceptable if the shed blood is not stored but is immediately reinfused.
Why are Witnesses so adamant about refusing blood products? If a transfusion is accepted, that person has abandoned the basic doctrines of the religion, and essentially separates themselves from it. They may then be shunned by other believers.
So what can trauma professionals do to provide best care while abiding by our patient’s religious belief? In trauma care it gets tricky, because time is not on our side and non-blood products are not necessarily effective or available. Here are some tips:
- Your first duty is to your patient. Provide the best, state of the art care you can until it is absolutely confirmed that they do not wish to receive blood products. In they are comatose, you must use blood if indicated until the patient has been definitively identified by a relative who can confirm their wishes with regard to blood. Mistaken identity does occur on occasion when there are multiple casualties, and withholding blood by mistake is a catastrophe.
- Talk with the patient or their family. Find out exactly what they believe and what they will allow. And stick to it.
- Aggressively reduce blood loss in the ED. We are not always as fastidious as we should be because of the universal availability of blood products. Use direct pressure or direct suture ligation for external bleeding. Splint to reduce fracture bleeding.
- Aggressively use damage control surgery. Don’t go for a definitive laparotomy which may take hours. Pack well, close and re-establish normal physiology before doing all the final repairs.
- Always watch the temperature. Pull out all the stops in terms of warming equipment. Keep the OR hot. Cover every bit of the patient possible with warming blankets. All fluids should be hot. Even the ventilator gases can be heated.
- Think about inorganic and recombinant products such as Factor VIIa, tranexamic acid and Vitamin K. These are generally acceptable.
- Consider angiography if appropriate, and call them early so their are no delays between ED and angio suite or OR and angio suite.
Bottom line: Do what is right for your patient. Once you are aware of their beliefs, avoid the use of any prohibited products. Speak with them and their family to clarify exactly what you can and cannot do. This is essentially an informed consent discussion, so make sure they understand the consequences. Follow their wishes to the letter, and don’t let your own beliefs interfere with what they want.