Most trauma patients
are considered to be at some risk for deep venous thrombosis (DVT) and/or
venous thromboembolism (VTE) during their hospital stay. Trauma professionals
go to great lengths to screen for, prophylax against, and treat these problems.
One of the tougher questions is, how long do we need to worry about it? For
fractures, we know that the risk can persist for months. But what about head
injury?
A group at Brigham
and Women’s Hospital did a large database study looking at the VTE risk in adults
who sustained significant head injury, with only minor injuries to other body
regions. They tried to tease out the risk factors using multivariate regression
models.
Here are the
factoids:
- Patients were only included if their AIS Head
was >3, and all other AIS were <3 - Of the over 50,000 patients in the study,
overall incidence of VTE was 1.3% during the hospital stay, and 2.8% overall
within 1 year of injury - Risk factors for VTE after discharge included
age > 64 (3x), discharge to a skilled nursing facility (3x), and prolonged
hospital length of stay (2x)
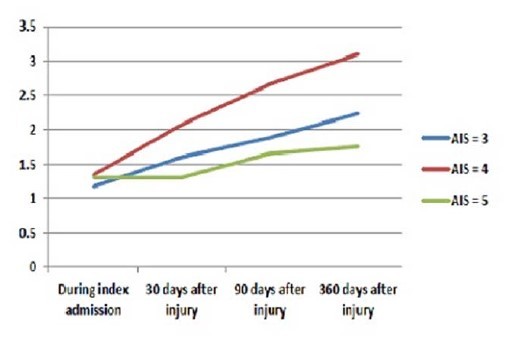
Incidence of VTE over time
Bottom line: View this paper as a glimpse of a potential unexpected
issue. The risk of VTE persists for quite some time after head injury (and
probably in most other risky injuries like spine and pelvic fractures. The
three risk factors identified seem to identify a group of more seriously
injured patients who do not return to their baseline soon after injury. We may
need to consider a longer period of screening in select patients, but I believe
further work needs to be done to help figure out exactly who they are.
Reference: How long should we fear? Long-term risk of
venous thromboembolism in patients with traumatic brain injury. EAST 2016 Oral
abstract #28.