There has been a tremendous amount of gnashing of teeth regarding venous thromboembolism (VTE) prophylaxis in patients with blood in their head. This means any kind of blood: subarachnoid / epidural / subdural hematomas as well as intraparenchymal hemorrhage.
Trauma professionals have traditionally been hesitant to give any type of anticoagulant to a patient who has just bled, or who may be at risk for bleeding in the very near future. This becomes even more important in areas like the brain where management is a bit more difficult and adverse events can be devastating.
For this reason, our neurosurgical colleagues frequently like to steer the ship and dictate what type of VTE prophylaxis can be given, and when. Unfortunately, much of their advice may be driven by dogma and what they learned about the subject during their training. Having studied hundreds of TQIP reports over the past few years, I’ve learned to pick out hospitals that are relying on the advice of non-trauma surgeons to direct the prophylactic regimen.
Here are two dead giveaways that something is amiss. First, look at your TQIP report table titled “Pharmacologic VTE Prophylaxis Type.”
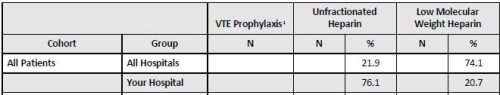
Compare the use of unfractionated heparin vs low molecular weight heparin (LMWH). This hospital has a huge variance from the norm compared to other comparable trauma centers. This means that “someone” is dictating its use for some subset of patients.
In my experience, this is typically a neurotrauma thing. Now take a look at the TQIP table titled “Pharmacologic VTE Prophylaxis.” Specifically, look at the “Severe TBI” cohort for time to VTE prophylaxis.
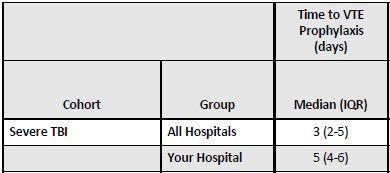
It is very clear that there is a significant delay to administering VTE prophylaxis to TBI patients. These two data points indicate that there is some reluctance to giving appropriate treatment to these patients.
The literature is clear that VTE prophylaxis is important in many trauma patients, including those with serious head injury. There are three questions that need to be answered to settle on optimal care:
- Which chemoprophylaxis is best, unfractionated or low molecular weight heparin?
- Is it better to give the selected agent earlier or later?
- If earlier is better, how early can we give it?
I will address each of these questions in this series of posts, focusing on neurotrauma patients. In order to try to toss out dogma, the literature I cite will be recent, no more than about two years old. So join me for battle next week as we have unfractionated vs low molecular weight heparin face off.
Thanks to Jim Sargent from Beth Israel Deaconess Medical Center for suggesting this topic.