Here is a list of practical tips for trauma professionals from prehospital and beyond:
- Apply supplemental oxygen from the get-go, in the field if possible
- Start an IV or IO and begin crystalloid infusion immediately
- Bump the patient to her left. This is most easily done with the spine board in place. Just put a rolled up towel under the right side of the board.
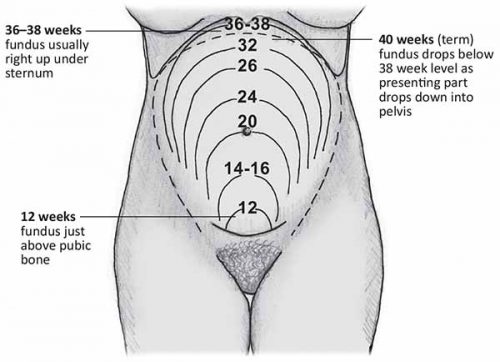
- Quickly estimate how pregnant the patient is if she can’t tell you. Use the fundal height diagram below. Key measurements to remember:
- Umbilicus = 20 weeks: entering the possible viability range if delivered emergently
- Xiphoid = approaching full term
- If the patient is 20 weeks+ pregnant, only transport to a trauma center (Level I or II).
- At the hospital, reassess fundal height to more accurately estimate viability
- If the fetus may be viable (23-24 weeks), call OB to the resuscitation area. But remember, they have nothing to offer until the trauma team secures the safety and stability of the mother. So don’t let them in the room until you have finished your entire evaluation. Nothing they can do (e.g. monitor) is helpful during the acute phase of the resuscitation.
- Once the mother is stabilized, assess fetal heart tones and apply monitors for fetal heart rate and maternal contractions.
- Add coag studies to your lab panel. Fetal and placental injury can cause clotting problems.
- Consider giving Rhogam in all major trauma cases if the mother is Rh negative
- Obtain a KB test to look at the amount of fetal blood in the maternal circulation. Why do this if you are going to give Rhogam anyway? Answer: sometimes the amount of fetal blood leakage is greater than that covered by a single vial of Rhogam.
- Plan your imaging intelligently. The next section covers this topic in more detail.
- If needed, chest tubes should be inserted 1-2 intercostal spaces higher than usual.
- The life-saving tetanus shot is safe in pregnant patients.